Categories
Change Password!
Reset Password!


A retrospective analysis was carried out to investigate the risk factors with the early predictive ability for severity and prognosis of severe acute pancreatitis (SAP).
The level of blood urea nitrogen within 24 hours after admission to the hospital was an independent risk factor for 30-day all-cause mortality in people suffering from severe acute pancreatitis.
Overall, 249 patients suffering from SAP were recruited and used as a training cohort. Participants were divided into 2 arms: (1) Survival arm (n=198), and (2) Mortality arm (n=51). To assess a 30-day survival if the hospital stay of a patient was less than 30 days, a follow-up via telephone was carried out.
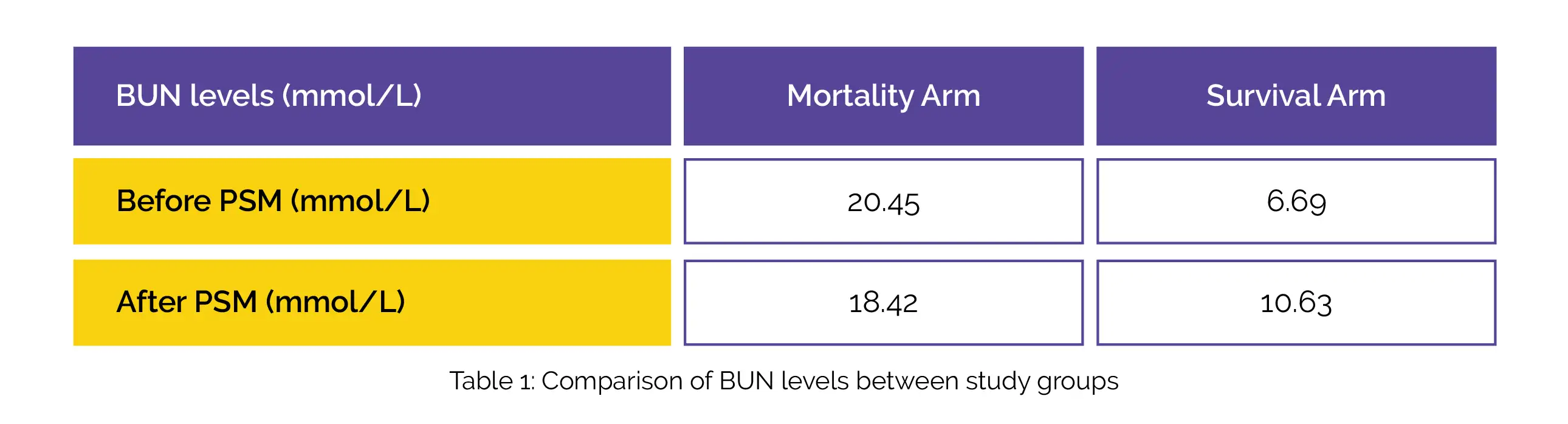
At 30-day post-admission, the all-cause mortality rate was 25.8% (51/198). In the mortality arm, the level of blood urea nitrogen (BUN) was remarkably higher compared to the survival arm before as well as after propensity score matching (PSM), as depicted in Table 1.
Notably, 0.820 was the area under the curve (AUC) of the receiver operating characteristic curve (ROC) of BUN. To predict 30-day all-cause mortality, the ideal BUN level cut-off came out to be 10.745 mmol/L. Additionally, SAP patients were segregated as per the BUN levels and graded based on the optimal cut-off value.
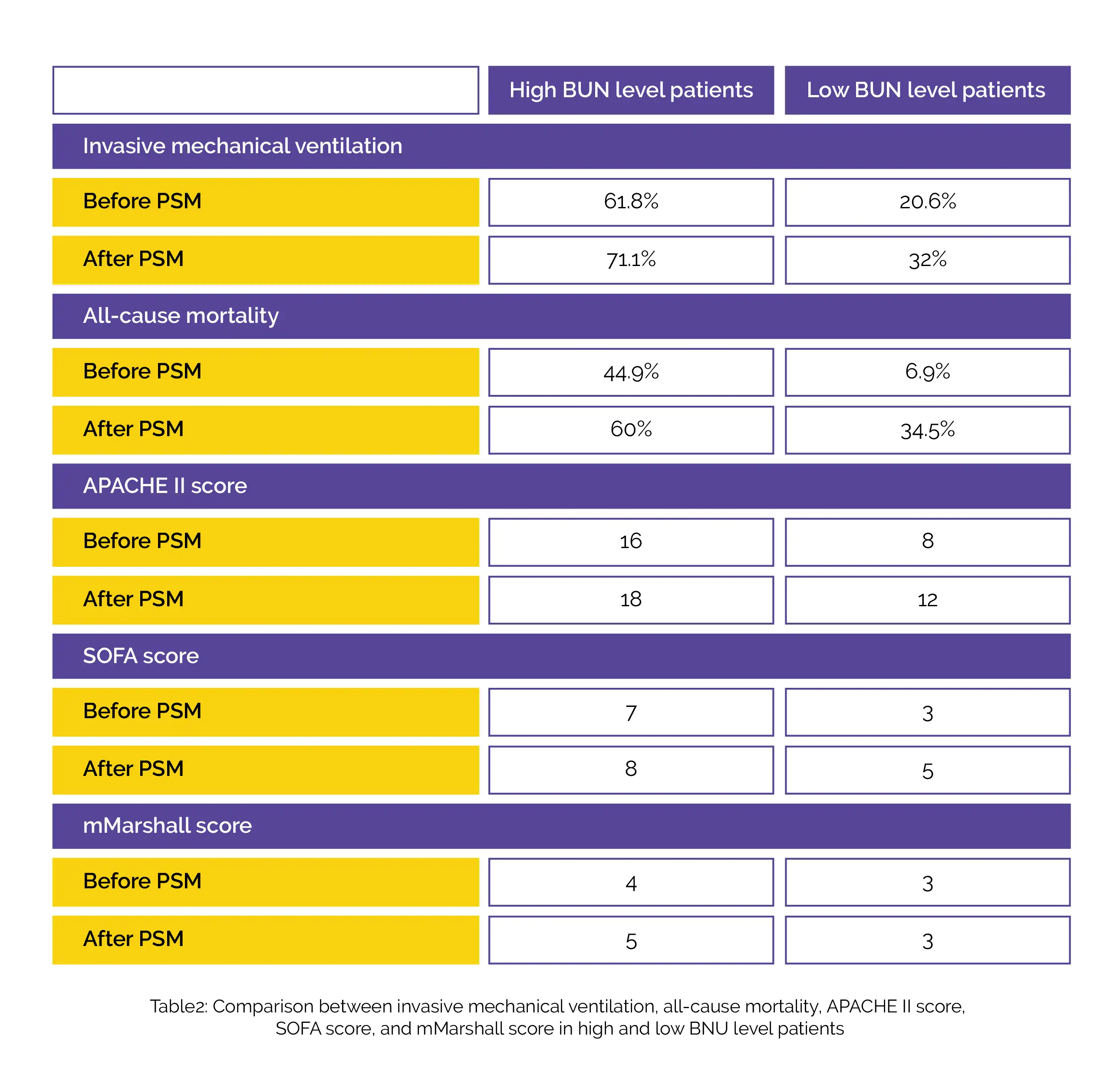
Higher rates of invasive mechanical ventilation and 30-day all-cause mortality, Acute Physiology and Chronic Health Evaluation (APACHE) II score, and modified Marshall (mMarshall) score, and Sequential Organ Failure Assessment (SOFA) score were observed in high BUN level patients compared to low BUN levels before as well as after PSM, as shown in Table 2.
Validation of BUN's efficacy as a prognostic marker was done utilizing ROC curves for external validation set (n = 49). Notably, the AUC of BUN was found to be 0.803 which depicted its capability to anticipate 30-day all-cause mortality in SAP people. A considerable rise in occupancy of the intensive care unit was seen in the high BUN level arm before PSM (93.3% vs. 73.1%), but not post-PSM (97.8% vs. 86.2%).
BUN level at admission is beneficial to predict 30-day all-cause mortality. An elevated BUN level is a reliable and meaningful predictor of early warning of SAP.
Disease Markers
Nitrogen
Minhui Dai et al.
Comments (0)