Categories
Change Password!
Reset Password!


In patients with sciatic radiculopathy, ultrasound-guided transgluteal sciatic nerve block effectively reduces pain.
An emergency department (ED)-performed transgluteal sciatic nerve block (TGSNB) has a good safety profile and has been linked to clinically meaningful pain decrease, enhanced mobility, and improved patient dispositions, according to a multicenter prospective research. Researchers aimed to assess the effectiveness and safety of ED-performed TGSNB for acute sciatic radiculopathy.
ED patients with acute sciatica were incorporated. Patients completed a brief questionnaire on therapies they had tried and their effects on work, performed a Timed Up & Go test (TUG), and rated their initial pain score (0–10) before receiving TGSNB. Prior to the block, providers were instructed to note the anticipated disposition for each patient. All TGSNBs were carried out by ED personnel who had gone through a 20-minute training course on the study protocol, block technique, and anatomy review.
For each TGSNB, 8 mg of Dexamethasone and 10 mL of 0.5% Bupivacaine were combined. At 15-30 minutes after the intervention, healthcare professionals noted each patient's final disposition, participants again reported their pain levels, and repeated the TUG test. The patients had a 72-hour post-intervention follow-up period, reported pain levels and self-reported ambulation status at several intervals. Using paired sample t-tests, longitudinal variables were contrasted to their pre-intervention values.
During the trial period, 46 ED TGSNBs were performed. A total of 32 subjects had provider measured dispositions, TUG tests, and complete pre- and post-block pain levels. During a 72-hour follow-up period, 16 subjects completed all pain scores and surveys regarding their ambulatory status. No complications (0/46) were recorded. In the 72 hours before their ED visit, 37.5% of the 32 subjects with complete periprocedural data reported being unable to work because of sciatica; 68% supported the use of NSAIDs; and 16% reported using opioids before arrival.
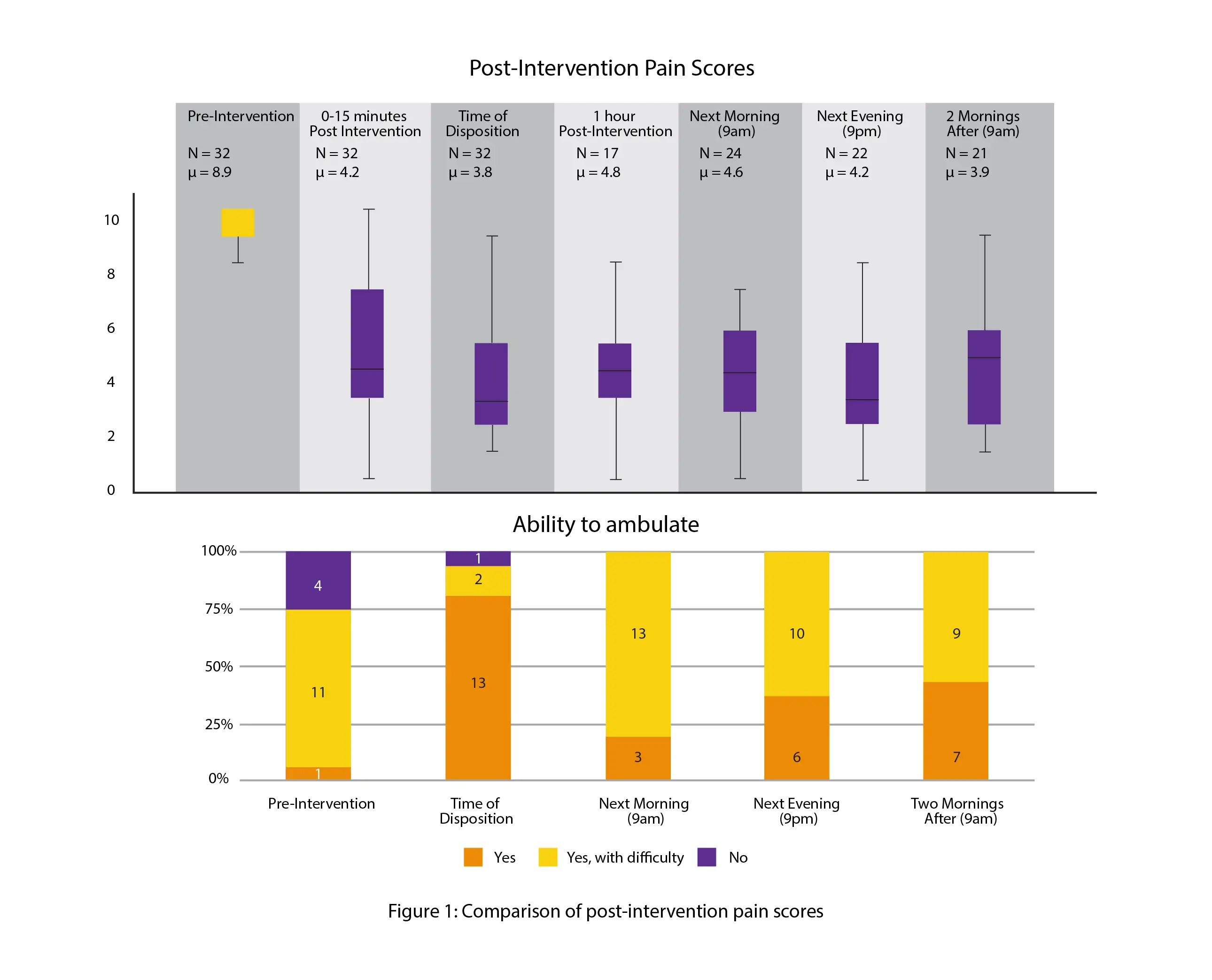
Notably, 15–30 minutes after the block, patients' numerical pain ratings (0–10) on average dropped by 4.72 points. For 71.9% (23/32) of the subjects, there was a post-block enhancement in TUG performance. However, for 25% (8/32) of the patients, there was no alteration in TUG performance, and for 3.1% (1/32) of the patients, there was a worsening of TUG performance. Before the TGSNB, physicians predicted that 50% (16/32) of subjects would need a hospital admission or observation unit. However, after the block, only 19% (6/32) of patients needed either. The findings of the pain and ambulation assessment conducted 72 hours after the block are shown in Figure 1.
TGSNBs carried out in the ED were safe and linked to clinically significant decrease in pain, increased mobility, and better patient dispositions. Additional research is necessary to clarify the patient-centered and systemic benefits of TGSNBs performed in the ED, including potential decreases in systemic opioid usage and dependence, sustained and enhanced pain control, avoidance of unnecessary hospital admissions, shorter length of stay in the ED, and rapid return to work.
Annals of Emergency Medicine
248 Ultrasound-Guided Transgluteal Sciatic Nerve Block in Emergency Department Patients With Sciatic Radiculopathy: A Multicenter Prospective Study
J. Herrala et al.
Comments (0)