Categories
Change Password!
Reset Password!


In women undergoing modified radical mastectomy, the addition of Ketorolac to Bupivacaine in pectoral nerve block extends the postoperative analgesia time without altering hemodynamics.
According to a randomized controlled clinical study, 30 mg of Ketorolac as an adjunct to Bupivacaine in the pectoral nerve (PECS) block extends the postoperative analgesia duration without impacting hemodynamics in women scheduled to undergo breast surgery. Researchers wanted to evaluate the duration and quality of analgesia by adding Ketorolac in the PECS block.
A total of 46 females (age 21–60 years old) who underwent modified radical mastectomies under general anesthesia were randomly assigned to 2 groups: (1) Control group that received Bupivacaine 0.25% alone for PECS block, and (2) Ketorolac group that received Bupivacaine 0.25% plus 30 mg of Ketorolac for the block.
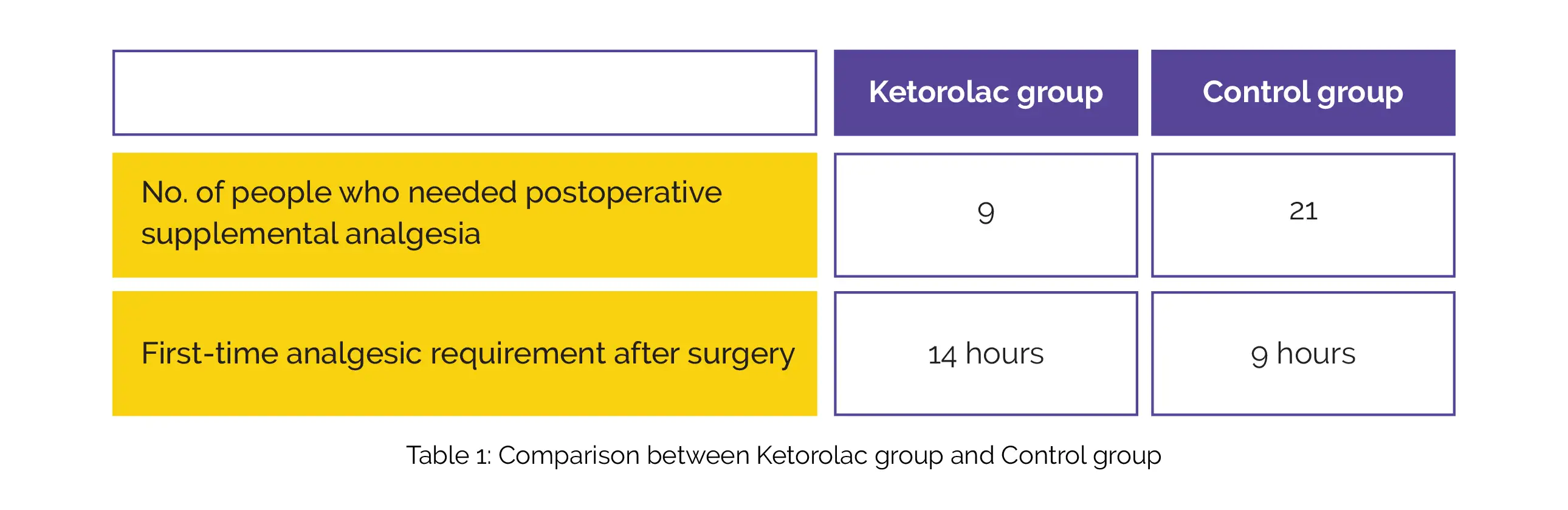
Compared to the control group, the number of subjects who required postoperative supplemental analgesia was profoundly lower and first-time analgesic requirement was substantially later in the Ketorolac group, as depicted in Table 1:
Hence, the duration of analgesia after surgery can be extended safely by adding Ketorolac to Bupivacaine in an ultrasound-guided PECS block.
Journal of Anaesthesiology Clinical Pharmacology
Analgesic effect of Ketorolac as an adjuvant to Bupivacaine in ultrasound-guided pectoral nerve block (I + II) for patients undergoing modified radical mastectomy: A Randomized controlled clinical trial
Al-Touny SA et al.
Comments (0)