Categories
Change Password!
Reset Password!


Migraine is a chronic neurological disorder that is accompanied by symptoms like vomiting, nausea, photophobia, and phonophobia.
In migraine patients, cognitive behavioral therapy effectively decreased headache frequency and migraine disability assessment (MIDAS) score.
Migraine is a chronic neurological disorder that is accompanied by symptoms like vomiting, nausea, photophobia, and phonophobia. It triggers severe headache and autonomic nervous system dysfunction (sweating, nasal stuffiness, facial flushing) and thus impacts the patients’ quality of life. Its prevalence is estimated to be 15–18%, and it is two to three times greater in females when compared to males.
Medication administration is the preferred treatment for migraine headaches. Triptans, paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs) are the commonly used acute medications for migraine. The routine usage of barbiturates and opioids is not preferred due to their poor tolerability and safety issues. Overusing painkillers can elicit numerous side effects and the vicious cycle of medication overuse headache. Thus, attention should be given to drug abuse during migraine treatment.
Along with medications, the non-drug therapy can be simultaneously used. This combination leads to a reduction in the occurrence of adverse effects. Doctors who treat migraine are gradually becoming more interested in complementary therapies. The common therapeutic options for migraine include flunarizine, antidepressants and hypertension treatments. For people with little response to existing drug therapies, pregnant females, and people with psychological disorders, acupuncture and biobehavioral therapy are also used to prevent migraine headaches.
Recently, nutritional supplements like cobalamin, riboflavin, vitamin D, pyridoxine, and folate have been extensively utilized as preventive therapies for migraine. In people with psychogenic neurological diseases, cognitive behavioral therapy have been reported to be beneficial to improve disability, pain, and emotional distress. In this therapy, cognitive factors are utilized for improving psychological distress and mental disorders.
The recent practice guidelines highlight cognitive behavioral therapy as selective psychotherapy for concerns ranging from personality disorders, anxiety, and depression to relationship pain, chronic pain, and addiction. For minimizing the frequency of migraine attacks and migraine-linked disorders, prior studies have shown the efficacy of behavioral therapy for migraine headaches, including cognitive behavioral therapy, biological feedback, and relaxation.
RATIONALE BEHIND RESEARCH
Though cognitive behavioral therapy has been utilized as a therapy for migraine attacks, there is only 1 systematic review on pediatric migraine, and no systematic review has been carried out on migraine patients of different age groups. Therefore, this study was carried out.
OBJECTIVE
A systematic review and meta-analysis were carried out to explore the safety and efficacy of cognitive behavioral therapy in patients with migraine.
Literature search
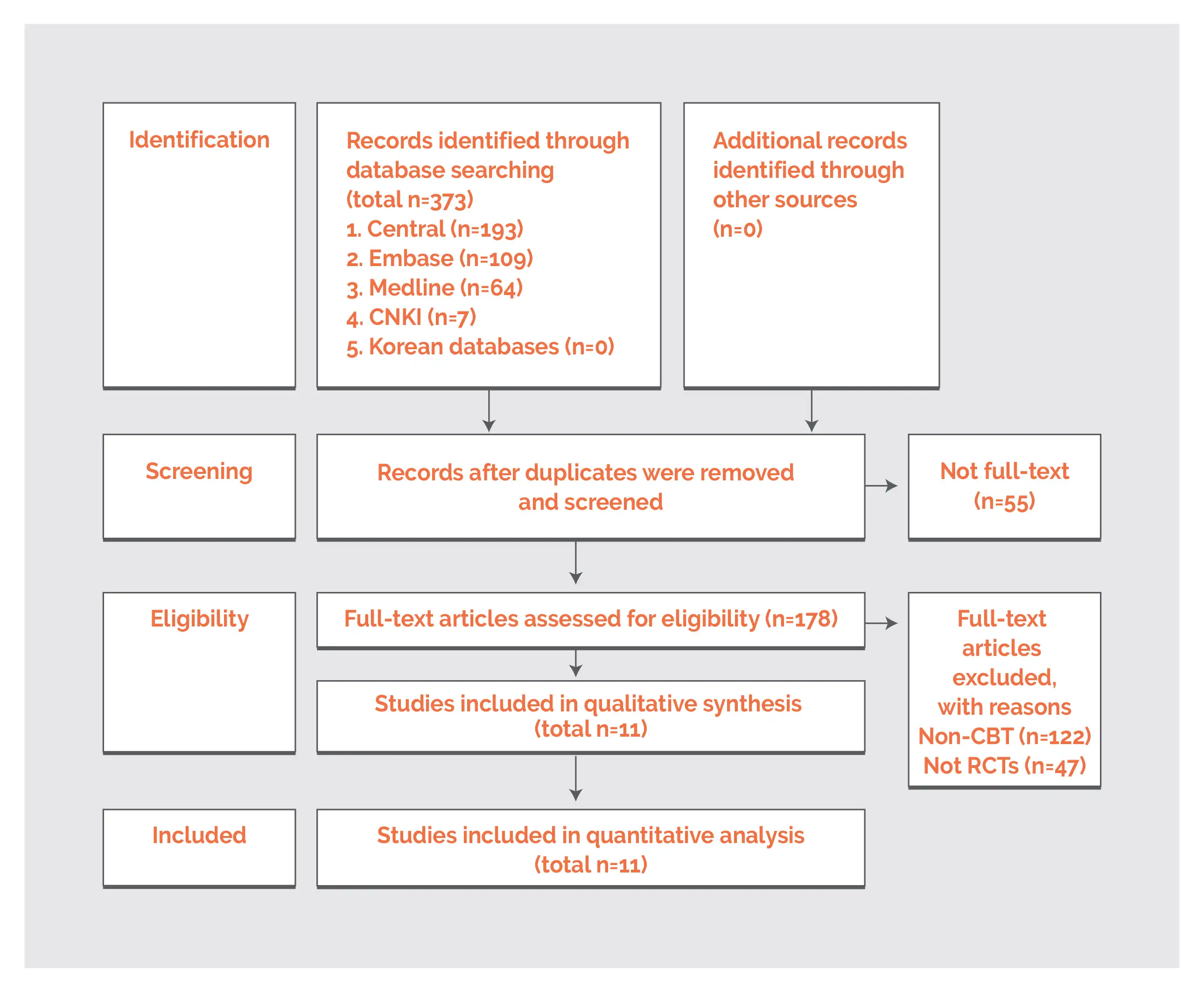
Chinese database (China National Knowledge Infrastructure), English databases (Cochrane Central Register of Controlled Trials, PubMed, Embase), and Korean databases (Research Information Service System, Oriental Medicine Advanced Searching Integrated System, Korean Studies Information Service System, National Digital Science Library, DBPIA) were explored to find out relevant randomized controlled trials (RCTs) that assessed the effectiveness of cognitive-behavioral therapy for migraine.
The search terms employed were “Cognitive behavioral therapy” and “Migraine”. As per the database, the search conditions were modified.
Inclusion criteria
Following studies were included in this systematic review:
Exclusion criteria
Study selection and Data extraction
The incorporated studies were evaluated by the study authors. A comprehensive assessment was performed by the authors with the help of an extraction form. This form included adverse effects, country, effect size, study design, age, gender, exclusion criteria, number of participants, inclusion criteria, duration, and outcome index. The endpoints of the study were evaluated at baseline, after therapy, and follow-up. In case of missing or unclear results, the authors of the incorporated studies were contacted.
Data and Statistical Analysis
For investigating improvement in migraine, the weighted mean difference and standard deviation of the major endpoints were estimated for meta-analysis using Review Manager and Cochrane Collaboration with 95% confidence intervals (CI). Researchers determined effect estimates with mean difference and standard deviation for continuous outcomes. Using I2 statistics, heterogeneity was evaluated.
Mostly, the fixed effect model was utilized. In case I2 was >75%, the random effect model was adopted for meta-analysis. The subgroup analysis was segregated as per the control group’s method. With the aid of I2 statistics, heterogeneity was determined. When heterogeneity was greater than 70%, the researchers carried out a subgroup assessment for explaining the source of heterogeneity with the aid of the Review Manager.
Risk of Bias and Quality assessment
For evaluating the quality of incorporated studies, the Cochrane risk of bias assessment tool was utilized. Each bias was categorized into high risk, low risk, and unclear risk and was examined by two investigators. Following domains were investigated: (I) allocation concealment, (ii) sequence generation, (iii) blinding of outcome evaluation, (iv) blinding of study volunteers and research personnel, (v) incomplete outcome data, (vi) selective outcome reporting, and (vii) other biases.
Study outcomes
Outcomes
Study and participant characteristics:
Study quality:
Effect of intervention on the outcome:
Migraine attacks vary in frequency and severity. This prevalent condition can substantially impair social, personal, and work life. Currently, the standard therapy for migraine headaches is taking medication. However, a psychiatric approach with a raised level of psychological co-prosperity has also drawn significant attention. People suffering from migraine are gradually approaching complementary and integrative health strategies.
Since people have an increased preference for cognitive behavioral therapy, numerous behavioral therapies for migraine prevention have been utilized, particularly during pregnancy or when pharmacological choices for people are limited, such as low efficacy or lack of durability in pharmacotherapy, or in combination with pharmacological therapies.
Cognitive behavioral therapy is defined as cognitive processes associated with the development and maintenance of psychopathology, especially emotional pain and dysfunction, that are mainly carried out during sessions. It allows people to develop preventive and acute care strategies, like trigger identification, physiological autoregulation strategies, and alteration of maladaptive interrelated thoughts, feelings and behaviours surrounding headache.
The behavioral therapies for migraine attacks, including cognitive behavioral therapy, biofeedback, and relaxation have shown effectiveness in decreasing the frequency of migraine attacks and migraine-associated disorders. Prior investigations have illustrated that cognitive behavioral therapy diminishes chronic pain and disability in people. This systematic review and meta-analysis investigated the effectiveness of cognitive behavioral therapy in migraine patients.
Consistent with the findings of the prior studies, this study demonstrated that cognitive behavioral therapy can remarkably decrease headache frequency and MIDAS scores. Only a few adverse events were reported. In a subgroup assessment of headache frequency, cognitive behavioral therapy effectively minimized migraine incidence rate in comparison with education alone. However, no profound difference was noted in headache frequency when compared to the wait-list/treatment as usual/standard medical care group.
In the evaluation of fixed-effect model, the heterogeneity was high at 81%. Therefore, it was assessed utilizing a random effect model for a more conservative assessment. In comparison with both education and wait-list/treatment as usual/standard medical care group, the MIDAS score in the subgroup assessment demonstrated substantial alteration. Furthermore, in the subgroup assessment with wait-list/treatment as usual/standard medical care, the HIT-6 score demonstrated considerable alteration.
For minimizing publication bias, the results of English, Korean and Chinese databases were screened.
For studies with only F value, the authors were contacted to procure the mean (standard deviation) value. Cognitive behavioral therapy showed promising benefits for migraine management (though the number of studies incorporated in this analysis is small). Additionally, it may be used as a complementary treatment for migraine patients.
Since cognitive behavioral therapy is getting considerable attention as an alternative to migraine management, more robust RCTs must be carried out for investigating efficacy of cognitive behavioral therapy + existing standard treatments for the management of people suffering from migraine.
In people with migraine, cognitive behavioral therapy exhibits remarkable effects in terms of alleviation of disability. In clinical practice, it appears to be a promising option to decrease disability elicited by migraine attacks.
Medicina
Cognitive Behavioral Therapy for Migraine Headache: A Systematic Review and Meta-Analysis
Ji-yong Bae et al.
Comments (0)