Categories
Change Password!
Reset Password!


Worldwide, esophageal cancer (EC) affects more than 570,000 individuals annually.
In individuals with Barrett's esophagus, the use of proton pump inhibitors is linked with a lower occurrence of high-grade dysplasia and esophageal adenocarcinoma.
Worldwide, esophageal cancer (EC) affects more than 570,000 individuals annually. EC claimed more than 500,000 deaths in 2018, placing it sixth in terms of cancer-related mortality and seventh in terms of occurrence. The rise in the prevalence of Barrett's esophagus (BE) is strongly correlated with the occurrence of esophageal adenocarcinoma (EAC). BE is a gastroesophageal reflux disease (GERD)-related metaplastic alteration in the lower section of the esophagus.
In GERD, an aberrant columnar epithelium with gastric and intestinal phenotypes replaces the stratified squamous epithelium. High-grade dysplasia (HGD), EAC, and low-grade dysplasia (LGD) are the stages of progression in BE. Even though modern surveillance and treatment methods have improved overall results, EAC still has a dismal prognosis that is worse than that of the majority of other cancer forms. The 5-year survival rate for EAC in patients from western populations is only 20%. Therefore, preventative intervention requires additional focus.
Statins, proton pump inhibitors (PPIs), and nonsteroidal anti-inflammatory drugs (NSAIDs) have a significant influence on the occurrence or risk of EAC in persons with BE, according to prior research. Among the aforementioned drugs, PPI exhibits the strongest acid-suppression ability. This makes PPI efficacious to reverse or slow the pathophysiological progression of BE in GERD patients. The usage of PPIs, however, may be linked to negative side effects, such as hypomagnesemia, dementia, fatty liver disease, cardiovascular disease, and fractures.
In addition, the controversy about whether PPIs can stop BE from developing into cancer always exists. Few studies showed an association between PPI use and a reduced risk of HGD/EAC, while some did not reach the same conclusions.
RATIONALE BEHIND RESEARCH
Prior investigation on the relationship between PPI usage and the risk of advancement HGD/EAC in BE patients has generated inconsistent findings. It is thus necessary to reevaluate the impact of PPI on preventing HGD/EAC among BE patients by conducting an updated meta-analysis considering its adverse effects, including hypomagnesemia, fatty liver disease, cardiovascular diseases, fracture, and dementia as well as controversial conclusions from prior meta-analyses.
OBJECTIVE
The goal of this meta-analysis was to clarify the relationship between the usage of PPIs and the likelihood that BE patients may develop HGD or EAC.
Literature search
In order to choose the most pertinent studies, a thorough search technique was used. Wanfang Data, VIP (Chinese) database, CNKI (China National Knowledge Infrastructure), CBM (China Biomedical Database), Web of Science, Cochrane Library, Embase, and PubMed were all explored.
(PPI" OR "PPIs" OR "proton pump inhibitors" OR "proton pump inhibitor" OR "Omeprazole" OR "lansoprazole" OR "dexlansoprazole" OR "esomeprazole" OR "pantoprazole" OR "rabeprazole" OR "acid suppress" OR "acid suppression") AND ("cancer" OR "carcinoma" OR "neoplasms" OR " “tumor” OR “adenocarcinoma” OR “metaplasia” OR “HGD” OR “High-Grade Dysplasia” OR “High-Grade Dysplasia”) AND (“oesophageal” OR “esophageal” OR “esophagus” OR “oesophagus”) AND (“Barrett’s esophagus” OR “Barrett esophagus” OR “Barrett’s oesophagus” OR “Barrett oesophagus”) were the terms that were utilized. Chinese phrases having the same meanings were utilized in the Chinese database.
Inclusion criteria
Studies were incorporated in this meta-analyses if:
Exclusion criteria
The following studies were excluded:
Study selection and Data extraction
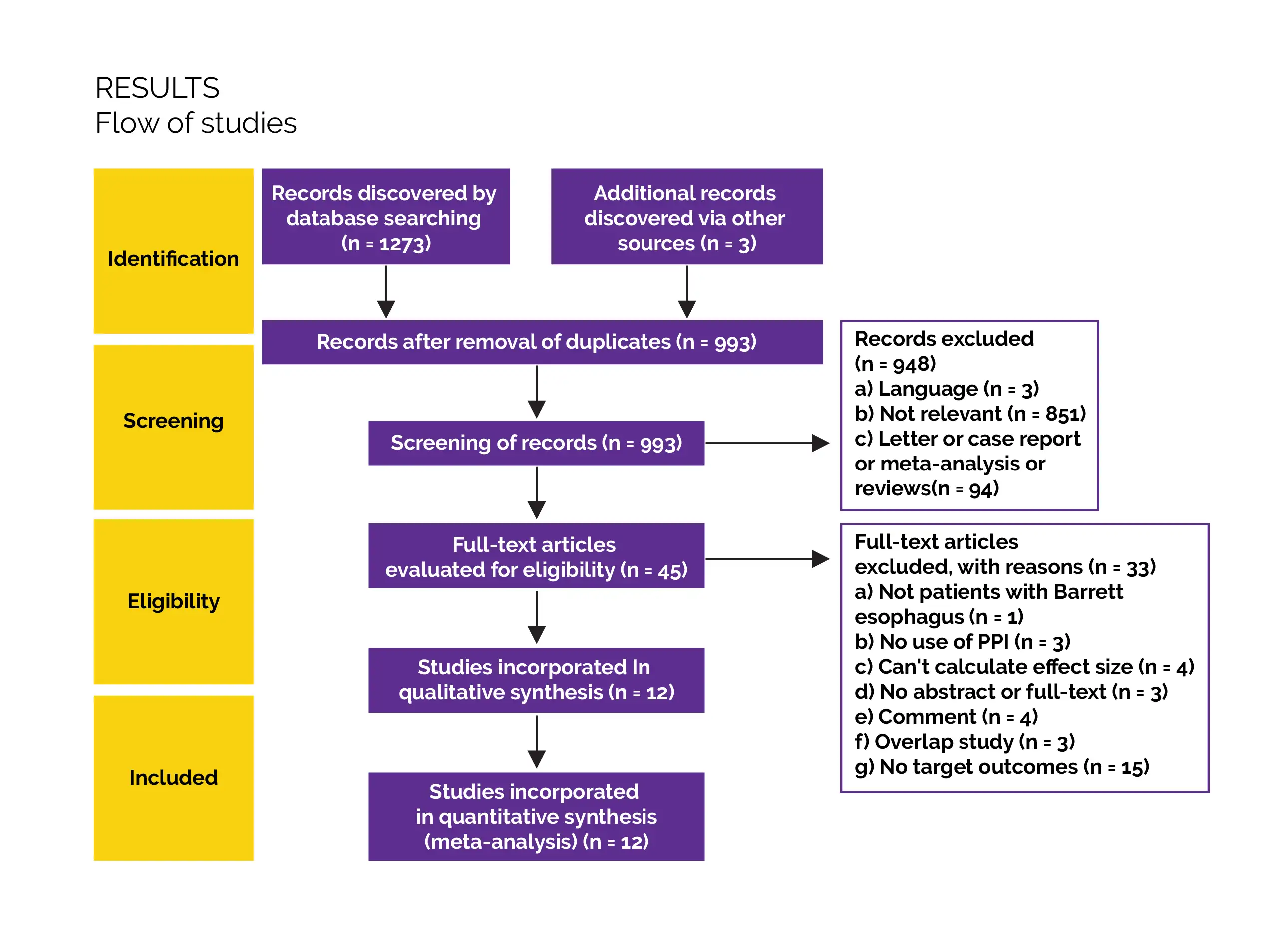
A total of 1276 records were eventually validated by electronic search. After eliminating redundant literature, reviewing the abstracts and titles, a total of 994 possibly relevant studies were finally selected. The inclusion criteria were fulfilled by twelve studies (out of forty-five studies). Data extraction and literature screening were carried out separately by two reviewers in accordance with the inclusion and exclusion criteria.
The reviewers discussed and resolved any differences or sought advice from a third researcher. Newcastle-Ottawa Scale (NOS) scores, adjusted confounders, the incidence of HGD/EAC, total number of patients with baseline dysplasia status, study period, length of PPI usage, nation, type of research, year, author etc. were all incorporated in the data extraction content.
Data and Statistical Analysis
The inverse variance approach was used to pool the adjusted ORs with 95% CIs of the included studies in order to assess the relationship between PPI usage and HGD/EAC outcomes. The absolute risk of HGD/EAC was relatively low. Hence, the HRs and RRs were anticipated to produce comparable estimates as ORs and were all pooled as ORs. When more than one effect value was offered in a single research, the one that most effectively controlled confounders was chosen. The I2 statistics and Q test were used to ascertain heterogeneity between the studies.
The Laird random-effects and Der- Simonian model was used to measure the pooled OR and 95% CIs when significant heterogeneity was found (I2 > 50%). In all other cases, fixed-effects model was employed. By altering the random-effects or fixed-effects models and deleting one research at a time, sensitivity analyses were carried out. According to the adjusted cofounders, sample size, study methodology, follow-up duration, and research location, subgroup analysis was carried out.
Using the approach of restricted cubic splines with four knots of the distribution in the glst module of Stata 14.0, the duration-response relationship was noted between the length of PPI usage and risk of HGD/EAC. A P value < 0.05 was regarded as clinically meaningful for all statistical analyses, which were carried out using STATA 14.0 statistical software and RevMan programme.
Risk of Bias and Quality assessment
With the aid of visual inspection of the funnel plot, Egger's test, and Begg's test, publication bias was examined. To evaluate quality of incorporated studies, 2 writers independently used the NOS. If there was a difference of opinion, it was resolved by discussion or by getting a second opinion. The NOS scale is especially useful for scoring observational studies.
Cohort studies were assessed in terms of selection, comparability, and outcome, whereas case-control studies were assessed in terms of selection, comparability, and exposure. It contains 8 items and a maximum score of 9 stars. Furthermore, documents with seven stars or more were seen to be of good quality, whereas those below seven stars were thought to be of lower quality.
Study outcomes
The primary outcome was PPI's impact on prevention of HGD/EAC among BE patients
Outcomes
Study and participant characteristics:
Study quality:
Effect of intervention on the outcome:
The use of PPIs slows BE progression to HGD/EAC, according to this meta-analysis that included 5 case-control and 5 cohort studies. The findings of the prior meta-analysis (Hu et al. 2017) of PPI usage and the progression to HGD/EAC, where different inclusion criteria were used, were inconsistent with this outcome. In the research by Hillman et al., the study group used PPI (delayed) when compared to the blank control group (non-PPI). However, rather than focusing on delayed PPI usage, this meta-analysis and the one before (Hu et al. 2017), focused on PPI use for progression.
Even though the outcome under the inclusion criteria of the previous meta-analysis conducted by Hu et al. was occurrence of HGD/EAC and not any degree of dysplasia, it encompassed the research carried out by Altawil et al., whose outcome index was some degree of dysplasia or EAC. Non-invasive carcinoma (carcinoma in situ) and high-grade adenoma/dysplasia are both categorized as category 4, by the Vienna classification of gastrointestinal epithelial neoplasia, necessitating endoscopic or surgical local resection, comparable to the approach used to treat early-stage EAC.
The authors included only those studies that reported HGD/EAC. Since the study carried out by Altawil et al. reported some degree of dysplasia or EAC rather than HGD/EAC, therefore it was eliminated. The follow-up length of 5 years or less was related in the subgroup analysis with a 35% reduction in progression from BE to HGD/EAC, while the follow-up period of 5 years or more did not demonstrate the same connection. This was witnessed to be consistent with the outcomes of study performed by Hu et al.
Cohort studies revealed a favorable connection in terms of research designs, however case-control studies did not. Case-control studies are inherently biased (selection bias and recall bias), and it is challenging to determine the sequence of exposure and disease because of the fundamental difference between case-control studies and cohort studies. Furthermore, compared to the case-control studies included, the cohort studies included were of better quality. Cohort study findings were, therefore, more trustworthy than case-control study findings.
Additionally, the results were significant in both groups in the stratified analysis by sample size, and little heterogeneity was seen in groups with more than 1,000 participants. The subgroup of studies that was age-gender-adjusted, multivariable-adjusted, or unadjusted all showed protective benefits of PPI usage in the subgroup analysis stratified by adjusted confounders. Similar to the finding in the research by Singh et al., the adjusted multivariable included the contemporaneous use of aspirin and statins, offering some indication that the impact of PPIs might be independent of statin/aspirin usage.
Preclinical studies support the positive effects of PPIs and the possibility of progression of BE to HGD/EAC progression. PPIs are a class of inhibitors used to treat conditions caused by excess acid in the body, and they include pantoprazole, lansoprazole, omeprazole, and others. Prolonged duration of acid-suppressive effect, excellent specificity, and strong acid suppression are some of the benefits of PPIs. The proton pump in the parietal cells promotes the exchange of H+ and K+ in the tubules, which is the final stage of gastric acid production. It is well-known that PPIs suppress H+ and K+- ATPase. This, in turn, impedes the last channel of stomach acid secretion.
BE is the last stage in the normal course of GERD. In the United States, GERD affects around one-fifth of the population. According to estimates, 10% of people with gastroesophageal reflux are also diagnosed with BE. BE, which is the sole known precursor for EAC and is characterized as salmon-colored mucosa extending ≥ 1 cm from the gastroesophageal junction, can develop into HGD and then EAC. The additional harm of acid exposure at the metaplastic epithelium is lessened by lowering gastroduodenal reflux when the normal squamous epithelium is replaced by metaplastic intestinal-type columnar epithelium.
PPI can therefore aid in esophageal mucosa repair by minimizing acid exposure. PPI can directly interact with neutrophils and monocytes to provide anti-inflammatory effects in addition to its antisecretory actions. As a result, it lessens esophageal irritation and stops epithelial cells from developing into cancerous cells. This is in line with both the overall finding of a reduced occurrence of HGD/EAC in BE patients using PPIs and the findings of a duration-response analysis, which showed the risk of HGD/EAC lowers with varying PPI use durations.
For every medicine, there is often a critical dosage. The two typical medication dosages were detailed in this study. At 40 mg/day, pantoprazole is successful in treating H. pylori and ulcers. At 20 mg/day, it not only successfully prevents inflammatory lesions during hospitalization, but it is also readily available at lower doses. Omeprazole oral tablets, 20-40 mg once a day, are necessary for people with severe GERD symptoms or erosive esophagitis. Regarding bile reflux, prior research indicated that biliary reflux management may impede the transition from metaplasia to adenocarcinoma; nevertheless, it was debatable if PPIs had an impact on the cessation of biliary reflux.
While Dellon et al. (2010) came to the conclusion that bile reflux can exacerbate acid reflux-stimulated erosive esophagitis and cause PPI-refractory reflux symptoms without acid exposure, other studies have suggested that PPIs can significantly shorten the amount of time that bile reflux lasts in GERD patients even when bile reflux is not reduced to the normal range. According to some studies, long-term PPI usage may enhance gastrin synthesis, which may encourage cell growth and COX-2 expression, leading to the development of EC.
Long-term PPI usage has also been linked to hypomagnesemia, fatty liver disease, cardiovascular illnesses, fractures, and dementia. As a result, extended PPI usage to avoid HGD/EAC in individuals with BE requires particular vigilance to balance the advantages against the potential adverse effects.
The benefits of this meta-analysis should be emphasized despite its drawbacks. First, there were 19,828 volunteers in this meta-analysis. This huge sample size offered stronger support for the meta-analysis.
Second, this meta-analysis' inclusion criteria were more stringent than those of the previous one, guaranteeing the quality of the study. Third, stratification in this meta-analysis involved adjusted cofounders, sample size, research location, study design, and follow-up length. Fourth, a duration-response analysis was carried out. The majority of studies employed multivariable-adjusted ORs to produce the pooled OR indicators, which improved the accuracy of the research findings.
In summary, PPI usage is linked to a considerably lower probability of progression to HGD/EAC in BE patients. PPIs' protective effects appeared to be unaffected by the use of aspirin, statins, NSAIDs, age, drinking, smoking, and other confounding variables. Chemo-preventive drugs may be the best treatment option given the high occurrence of HGD/EAC in BE patients and the significant mortality of EAC.
To fully understand the preventive impact of PPI use on BE patients to avoid HGD/EAC, further well-designed studies from a variety of demographics are required. These robust studies may include randomized controlled trials and prospective cohort studies with large sample numbers, high quality, and extended follow-up periods.
PPIs may be used to reduce the progression risk of BE to HGD/EAC and thus appears to be beneficial for the management of people diagnosed with BE.
Journal of Cancer Research and Clinical Oncology
Do proton pump inhibitors prevent Barrett’s esophagus progression to high-grade dysplasia and esophageal adenocarcinoma? An updated meta-analysis
Yue Chen et al.
Comments (0)