Categories
Change Password!
Reset Password!


A randomized controlled trial was conducted to assess the effectiveness (long-term and short-term) and safety profile of acupuncture in treating chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS).
In people with chronic prostatitis/chronic pelvic pain syndrome, acupuncture can efficiently alleviate symptoms, enhance the quality of life, and offer a reliable and safe therapeutic effect.
A randomized controlled trial was conducted to assess the effectiveness (long-term and short-term) and safety profile of acupuncture in treating chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS).
A total of 42 subjects diagnosed with CP/CPPS were included in this study, and they were assigned randomly to two groups: an acupuncture group consisting of 21 volunteers (with one patient dropping out) and a sham acupuncture group consisting of 21 volunteers. In the acupuncture group, subjects received acupuncture treatment at specific acupoints, including bilateral Zhongliao (BL 33), Sanyinjiao (SP 6), Shenshu (BL 23), and Huiyang (BL 35). Shenshu (BL 23) and Sanyinjiao (SP 6) were punctured directly to a depth of 30 mm, while the depth of needling for Zhongliao (BL 33) and Huiyang (BL 35) was between 60 to 80 mm.
In contrast, the individuals in the sham acupuncture group received acupuncture treatment at locations that were non-acupoints. These non-acupoints included points 2 cm away from Huiyang (BL 35), Zhongliao (BL 33), and Shenshu (BL 23), as well as midpoints along the line connecting kidney meridian and spleen meridian. The acupuncture needles were inserted directly to a depth of 2 to 3 mm at these non-acupoint locations.
In both groups, the needles remained inserted for a duration of 30 minutes. This treatment schedule was followed for the initial four weeks, with sessions held every other day, and continued with a frequency of thrice a week for the subsequent 4 weeks, totalling 20 treatment sessions. The assessment involved the observation of urinary flow rate and the National Institutes of Health-Chronic Prostatitis Symptom Index (NIH-CPSI) score before treatment, post-intervention, and during a 24-week follow-up period following the completion of treatment. Additionally, clinical effectiveness and safety were determined throughout the study.
When comparing the scores before and after treatment, it was observed that both groups experienced a decrease in pain and discomfort scores, urination symptom scores, quality of life scores, and the total scores on the NIH-CPSI. Furthermore, in the acupuncture group, these scores continued to drop during the follow-up period.
Following the treatment and during the follow-up period, the acupuncture group exhibited lower scores for each individual item and the total score on the NIH-CPSI when compared to the sham acupuncture group. Additionally, post-treatment, there was an improvement in the maximum and average urinary flow rates within the acupuncture group, surpassing the rates observed prior to the treatment.
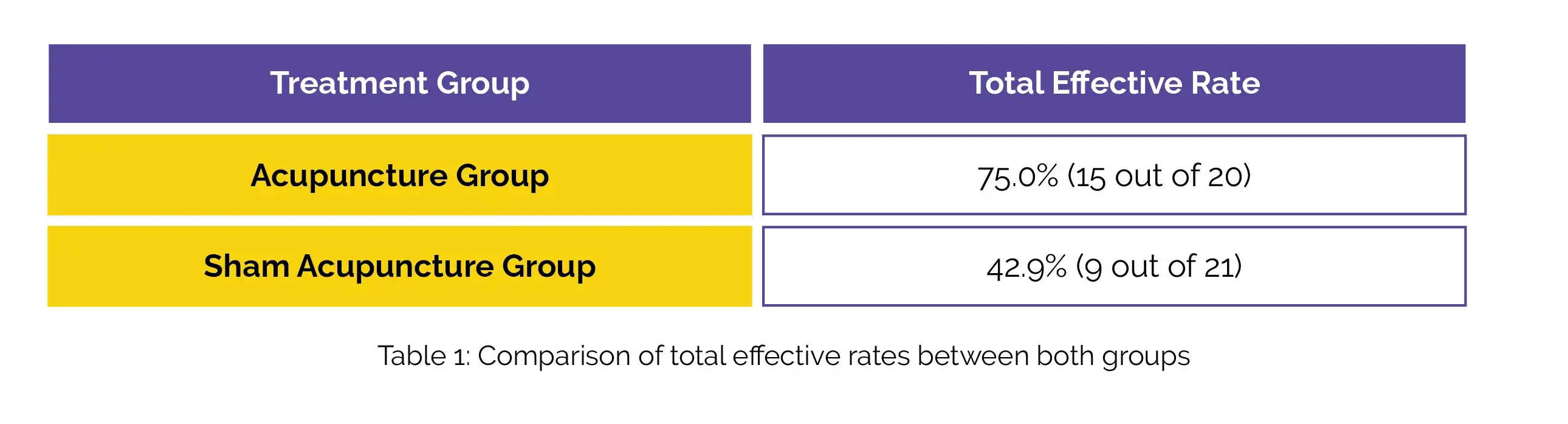
Moreover, the acupuncture group had a notably greater average urinary flow rate after the treatment in comparison with the sham acupuncture group. In the acupuncture group, the total effective rate surpassed that of the sham acupuncture group, as shown in Table 1.
No noteworthy adverse reactions were noted in either group, and the occurrence of adverse reactions did not show a substantial difference between both groups.
Acupuncture is a beneficial approach for addressing the needs of individuals experiencing CP/CPPS.
Chinese Acupuncture & Moxibustion
Acupuncture for chronic prostatitis/chronic pelvic pain syndrome: a randomized controlled trial
Bo Li et al.
Comments (0)