Categories
Change Password!
Reset Password!


A double-blind randomized trial was conducted to comprehensively analyse the effect of paravertebral block to prevent chronic pain after breast cancer surgery.
Paravertebral block may provide relief from postoperative pain among women who had undergone breast cancer surgery.
A double-blind randomized trial was conducted to comprehensively analyse the effect of paravertebral block to prevent chronic pain after breast cancer surgery.
A total of 380 female patients undergoing breast surgery were recruited and randomly categorised into two groups. 1) paravertebral group (group 1, n=178) which was administered with 0.35 ml/kg 0.75% ropivacaine and 2) control group (group 2, n=174) which was given saline. Both groups were administered with systemic multimodal analgesia.
The major outcome was chronic pain prevalence at three months after surgery with score of visual analogue scale > 3 out of 10. Anxiety, chronic pain at six and twelve months, neuropathic pain, nausea and vomiting, depression, analgesic consumption, acute pain and pain interference were the secondary outcomes.
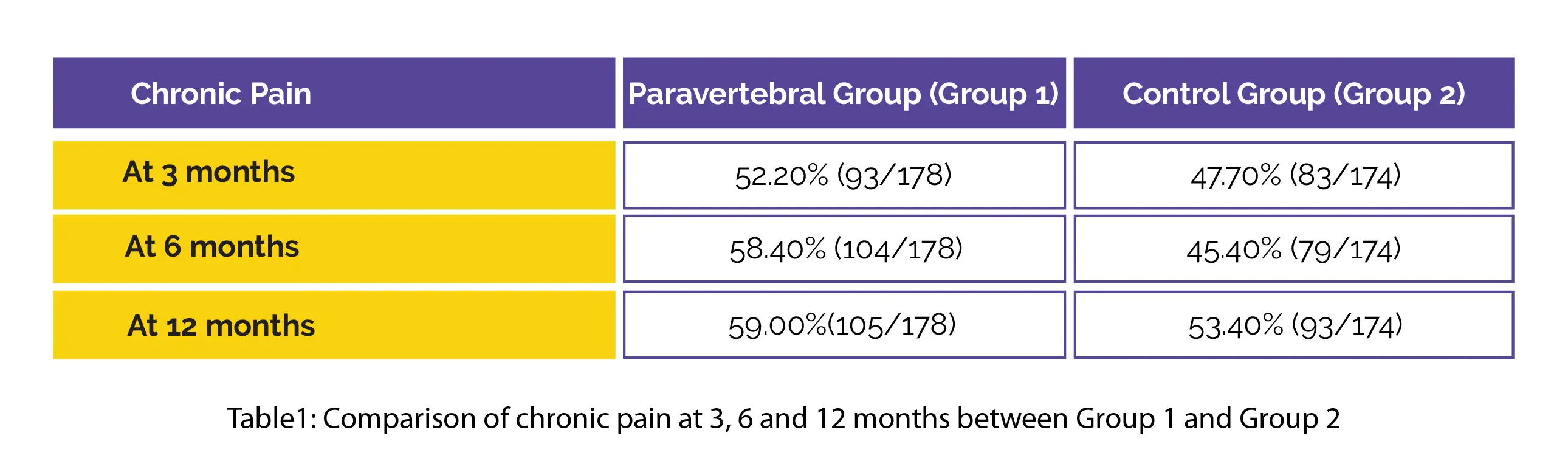
The incidence of chronic pain observed after 3, 6 and 12 months in both groups is illustrated in table 1.
Compared to the paravertebral group, the control group exhibited higher postoperative pain. The administration of post-surgery morphine was 73% reduced in the paravertebral group.
The incidence of chronic pain post-surgery was not lowered by paravertebral block but less immediate postoperative pain was seen. No other considerable differences were observed in postoperative outcomes.
Anesthesiology
Preoperative Paravertebral Block and Chronic Pain after Breast Cancer Surgery: A Double-blind Randomized Trial
Aline Albi-Feldzer et al.
Comments (0)