Categories
Change Password!
Reset Password!


Thoracoscopic surgery is extensively utilized for the treatment of several diseases like lung cancer and esophageal cancer.
Dexmedetomidine supplementation is beneficial to enhance the analgesic efficacy for thoracoscopic surgery
Thoracoscopic surgery is extensively utilized for the treatment of several diseases like lung cancer and esophageal cancer. Compared to traditional surgery, thoracoscopic surgery leads to minimized recovery duration, decreased pain and inflammatory response, and smaller incisions. Postoperative pain is common and exerts a detrimental effect on postoperative recovery. Several analgesic regimens that include regional and pharmacologic interventions (for example nerve block) have been created to manage pain that occurs after thoracoscopic surgery.
Dexmedetomidine is a short-acting α2 -adrenoceptor agonist that offers analgesia and sedation for numerous surgeries. Research has indicated that dexmedetomidine is safe and effective to enhance the analgesic efficacy when serving as an adjunctive analgesic. It also reduces the surgical stress responses in people undergoing surgery. Previous trials depicted that dexmedetomidine is beneficial for pain mitigation, minimized analgesic-related adverse events, and exhibited opioid-sparing features.
RATIONALE BEHIND RESEARCH
For thoracoscopic surgery, the effectiveness of dexmedetomidine supplementation has not been well-documented. Numerous studies have been published. However, the findings were contradictory. Therefore, this study was carried out to explore the analgesic efficacy of dexmedetomidine supplementation for thoracoscopic surgery.
OBJECTIVE
This systematic review and meta-analysis aimed to investigate the influence of dexmedetomidine on thoracoscopic surgery
Literature search
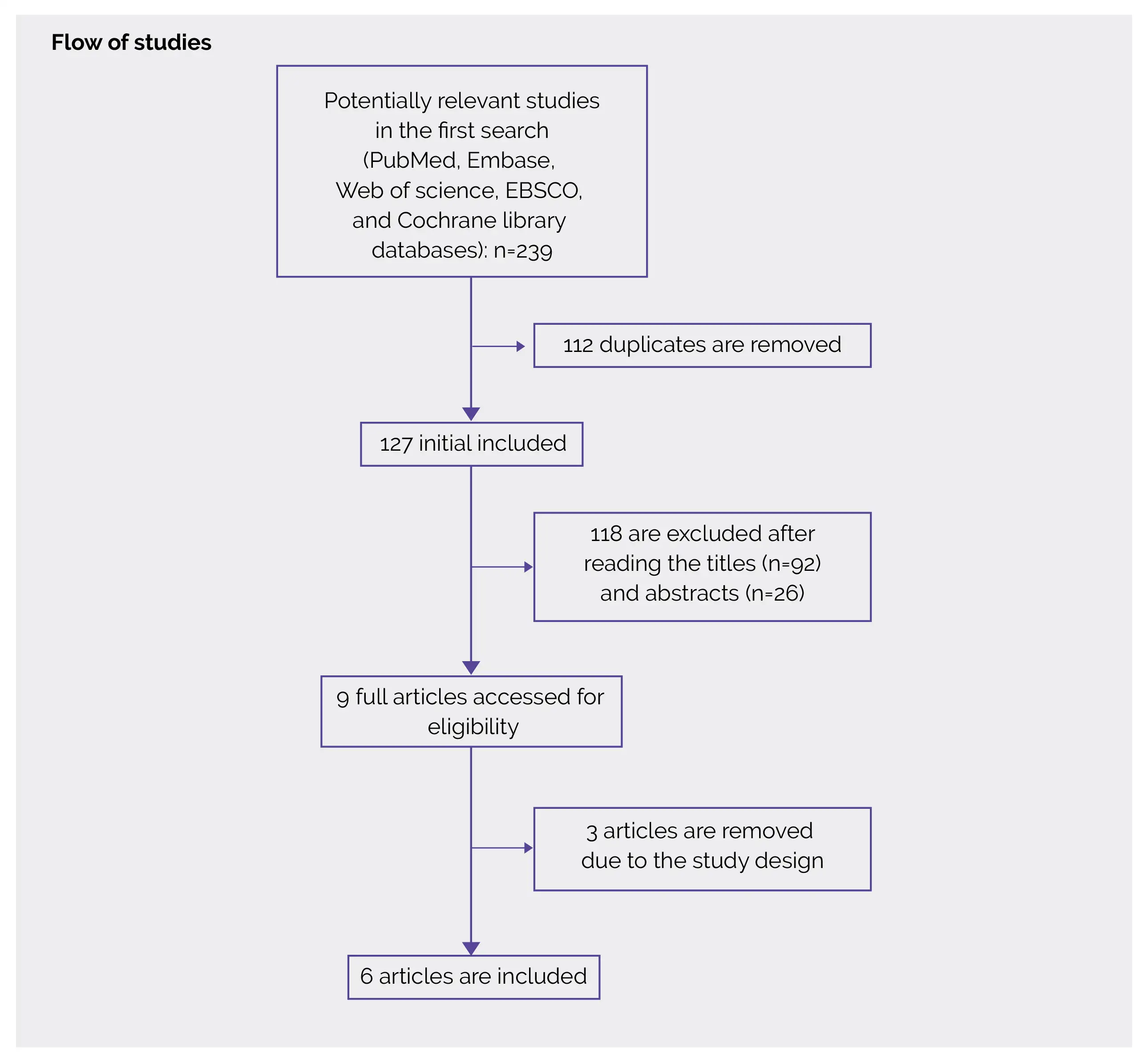
With the aid of databases such as Cochrane Library, EBSCO, Web of Science, Embase, and PubMed, the literature search was performed. Using the keywords “dexmedetomidine”, and “thoracoscopic” or “thoracoscopy”, the electronic search strategy was performed. The reference lists of screened full-text studies were also verified to find out other eligible trials.
Inclusion criteria
Studies were included in this systematic review if:
Study selection and Data extraction
Articles meeting the inclusion criteria were retrieved. Extraction of the information like body mass index, sex, age, number of patients, author, American Society of Anesthesiologists (ASA) and detail methods in each group was done. To describe a patient’s preoperative medical condition, the ASA Physical Status Classification System is extensively used. Data extraction was performed independently by 2 researchers and contradictions were solved by agreement.
Data and Statistical Analysis
For continuous outcomes (hospital stay, blood pressure, mean heart rate, analgesic consumption, and pain scores), the standard mean difference (SMD) with 95% confidence interval (CI) was assessed while for dichotomous outcomes (intensive care unit [ICU] stay), the relative risk with 95% CI was estimated. The utilization of the random-effects model was done irrespective of heterogeneity. Notably, I2 > 50% indicated significant heterogeneity that was reported using the I2 statistic.
Possible heterogeneity sources were searched by excluding 1 study in turn for meta-analysis or executing subgroup analysis whenever profound heterogeneity was present. Utilizing the Review Manager Version 5.3, all the statistical analyses were executed.
Risk of Bias and Quality assessment
Evaluation of the publication bias was not done due to the confined number (< 10) of incorporated studies. Utilizing the Jadad scale (score varies from 0 to 5 points), the methodological quality of the incorporated studies was independently investigated. In total, there are three items for the Jadad scale: (a) dropouts and withdrawals (0-1 points), (b) blinding (0-2 points), and (c) randomization (0-2 points). An article with a Jadad score ≤2 was deemed to be of low quality while an article with a Jadad score≥3 was deemed to be of high quality.
Study outcomes
Outcomes
Study and participant characteristics:
Study quality:
Effect of intervention on the outcome:
For the treatment of lung cancer, thoracoscopic surgery has been broadly utilized due to its minimal invasion, decreased hospital stay, and minimized postoperative pain when compared to open thoracotomy. For anesthesiologists and patients, the postoperative pain management, specifically early postoperative pain, yet remains a significant area of concern. Opioids are important during surgery. However, owing to the occurrence of adverse events like respiratory depression, opioid-elicited nausea, and delayed recovery from general anesthesia, various methodologies are prepared to lower opioid intake.
The use of intraoperative dexmedetomidine has been reported to enhance postoperative analgesic effects. It depicted anxiolytic, sedative and pain-relieving effects, and prevented respiratory depression and the suppressive effect of sympathetic stimulation as an adjuvant to general anesthesia. This meta-analysis incorporated 510 patients and 6 RCTs. The findings exhibited that intravenous dexmedetomidine was linked to a considerable reduction in pain scores, anesthetic intake, the RR of ICU stay and mean heart rate following thoracoscopic surgery.
However, it did not impact hospital stay or mean blood pressure. Additionally, dexmedetomidine aided in decreasing the stress response and maintaining the cardiovascular system's stability. Both epinephrine and norepinephrine are lowered by intraoperative infusion of dexmedetomidine. Dexmedetomidine has hypnotic, anxiolytic, and analgesic effects and can reduce the release of catecholamines. There is considerable heterogeneity regarding the sensitivity analysis. There may be various reasons for heterogeneity.
Primarily, various methods and doses of dexmedetomidine supplementation may cause some bias. For example, dexmedetomidine was utilized prior to anesthesia or during operation. Secondly, dexmedetomidine was employed as the adjunct to various drugs like sevoflurane and oxycodone, which may lead to several analgesic effects. Thirdly, different surgeries elicit different intensities of pain that might influence the pooling results.
Intravenous dexmedetomidine was linked with a remarkable reduction in pain scores, anesthetic consumption, and the RR of ICU stay. Hence, clinicians should consider dexmedetomidine supplementation in patients who underwent thoracoscopic surgery, as supported by the findings of a recent analysis.
Journal of Cardiothoracic Surgery
Effect of dexmedetomidine supplementation for thoracoscopic surgery: a meta-analysis of randomized controlled trials
Chengjun Song et al.
Comments (0)