Categories
Change Password!
Reset Password!


Maternal milk has been linked to better neurodevelopmental outcomes for extremely preterm infants compared to preterm formula, but little is known about donor human milk.
Donor human milk offers similar neurodevelopmental outcomes for extremely preterm infants who receive minimal maternal milk at 22 to 26 months of age when compared to preterm formula.
Maternal milk has been linked to better neurodevelopmental outcomes for extremely preterm infants compared to preterm formula, but little is known about donor human milk. Researchers set out to find if nutrient-fortified, pasteurized donor milk offers similar benefits compared to preterm formula for neural development at 22 to 26 months of age.
In a double-blind, randomized clinical trial involving 483 extremely preterm infants (born under 29 weeks gestation or weighing less than 1000 g), researchers compared the effects of donor human milk versus preterm formula. Infants were assigned to receive either type of milk (239 in the donor milk group and 244 in the preterm formula group) from birth until 120 days of age, hospital discharge, or death.
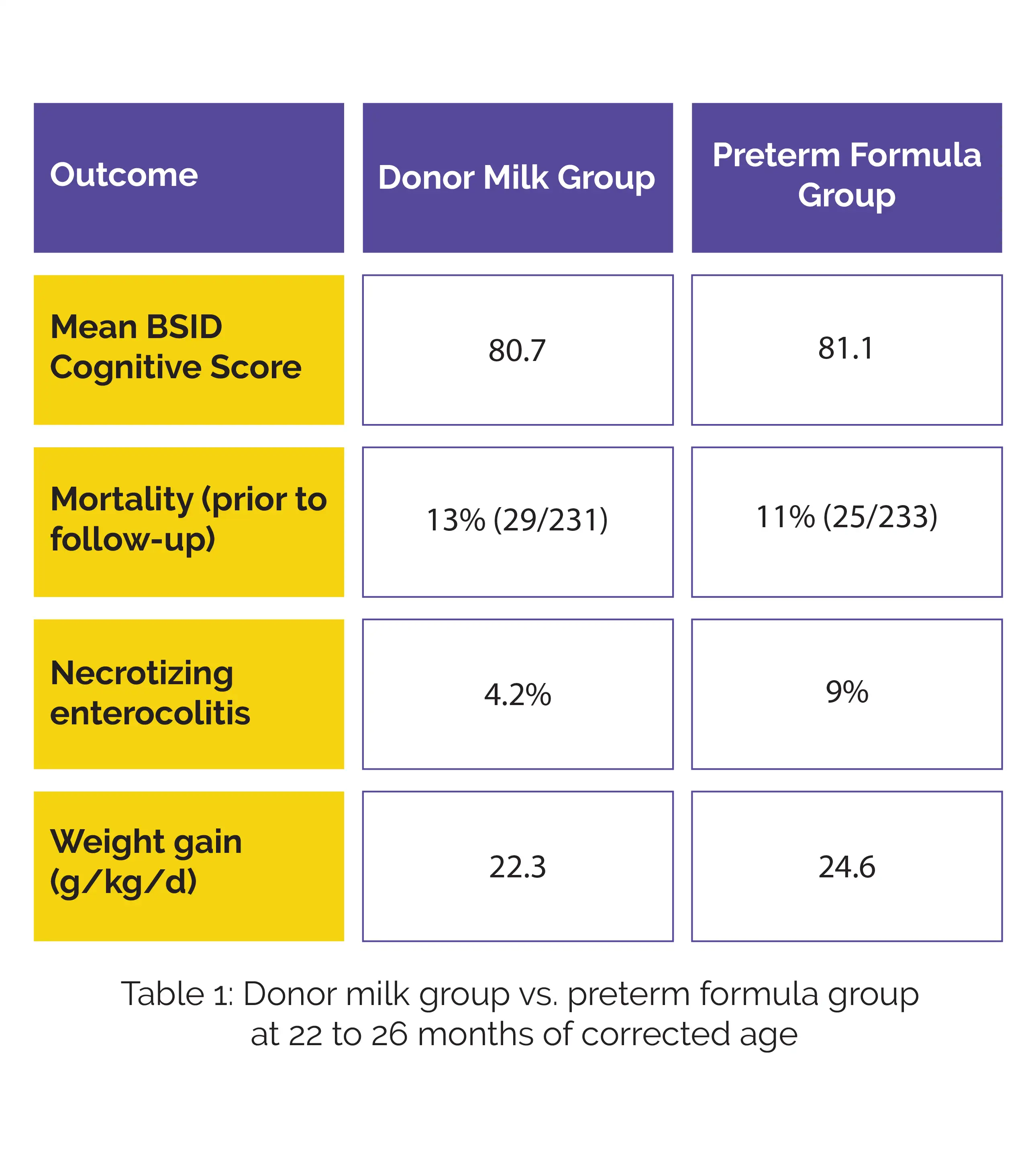
The key focus was on neurodevelopmental outcomes at 22 to 26 months of corrected age, estimated utilizing the Bayley Scales of Infant and Toddler Development (BSID) cognitive score. Secondary assessments included in-hospital growth, rates of necrotizing enterocolitis, mortality, and BSID language and motor scores.
The study found no vital differences in cognitive development between the donor milk group and the preterm formula group. Secondary endpoints, including BSID language and motor skills, were also similar between the study groups. Additional secondary outcomes, such as mortality, incidence of necrotizing enterocolitis, and weight gain, are detailed in Table 1 below.
For extremely preterm infants who received minimal maternal milk, donor human milk and preterm formula showed comparable neurodevelopmental outcomes.
JAMA
Neurodevelopmental Outcomes of Extremely Preterm Infants Fed Donor Milk or Preterm Infant Formula: A Randomized Clinical Trial
Tarah T Colaizy et. al.
Comments (0)