Categories
Change Password!
Reset Password!


A single-center, open-label, randomized controlled clinical study compared the patient compliance, cost, safety, and effectiveness of two rescue regimens (culture-based susceptibility-guided therapy [CB-SGT] and high-dose dual therapy [HDDT]) for H. pylori management.
For H. pylori-infected individuals with a history of unsuccessful therapy, high-dose dual therapy exhibits similar effectiveness at a reduced cost and with fewer side effects when compared to culture-based susceptibility-guided therapy.
A single-center, open-label, randomized controlled clinical study compared the patient compliance, cost, safety, and effectiveness of two rescue regimens (culture-based susceptibility-guided therapy [CB-SGT] and high-dose dual therapy [HDDT]) for H. pylori management.
Overall, 146 subjects who previously had elimination failure were recruited and randomly allocated to get HDDT or CB-SGT. Esomeprazole 20 mg and Amoxicillin 750 mg both administered 4 times per day (qid) were included in HDDT. Esomeprazole 20 mg two times a day (bid), Amoxicillin 1000 mg bid + Clarithromycin 500 mg bid, Metronidazole 400 mg bid, or Levofloxacin 500 mg daily (qd) for the sensitive individuals, were included in CB-SGT.
A bismuth-containing regimen combining a raised dosage of Metronidazole with Esomeprazole 20 mg bid, Bismuth 220 mg bid, Amoxicillin 1000 mg bid, and Metronidazole 400 mg qid was selected for patients who had triple resistance. All the regimens were prescribed for fourteen days.
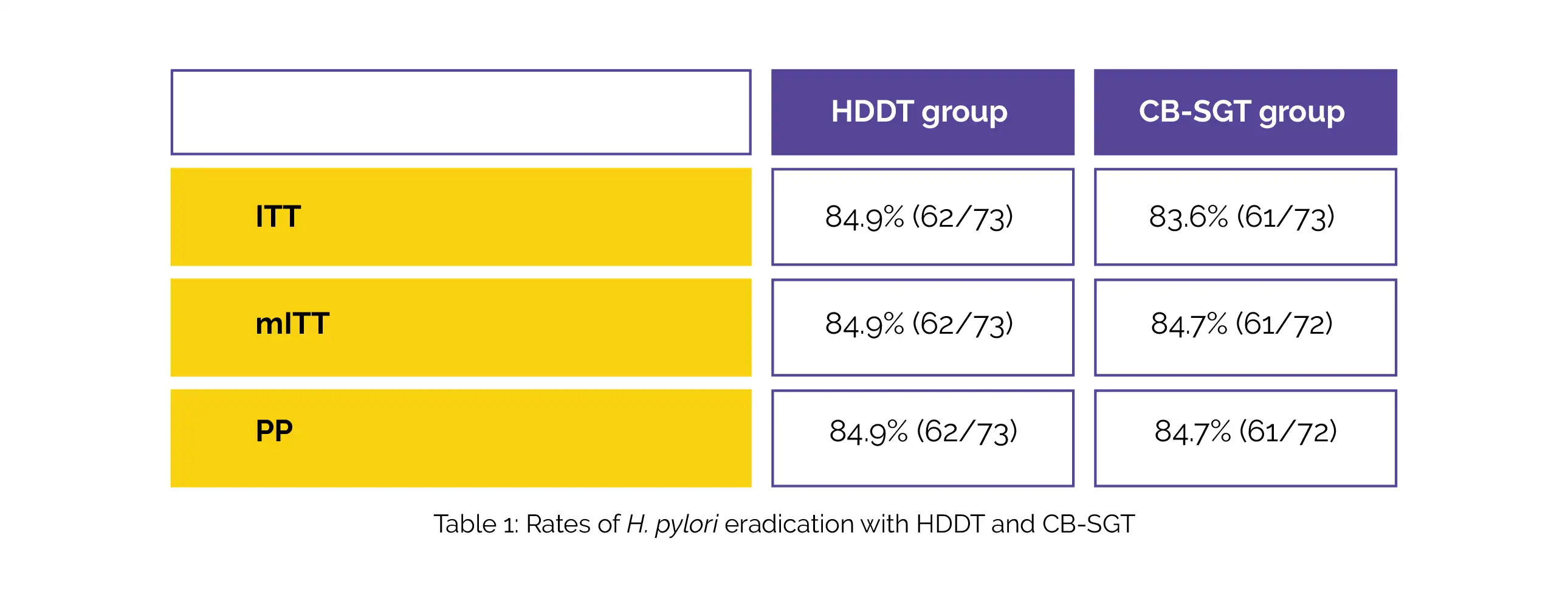
The H. pylori eradication rates achieved with HDDT and CB-SGT in the intention-to-treat (ITT), per-protocol (PP), and modified ITT (mITT) analyses are depicted in Table 1:
The eradication rates for HDDT and CB-SGT in patients with intermediate/poor CYP2C19 polymorphisms were 90.70% (39/43) and 84.21% (32/38), respectively. The non-inferiority p-value was 0.0128, and the difference between the study groups was 6.49%.
The two regimens' eradication rates for patients with treatment intervals longer than three months were 88.71% and 71.97% for HDDT and CB-SGT respectively. The non-inferiority p-value and the difference between the groups were 0.0042 and 6.74%, respectively. In both groups, there was high patient adherence. When compared to CB-SGT, the HDDT was less expensive and exhibited fewer side effects.
With strong adherence, fewer side effects, reduced costs, and less usage of antibiotics, HDDT can achieve an elimination rate of 85% in treatment-experienced people having H. pylori infection and 91% in people having CYP2C19 polymorphisms of poor/intermediate metabolizers. Hence, HDDT can serve as an efficient rescue regimen for H. pylori eradication.
Therapeutic Advances in Gastroenterology
High-dose dual therapy versus culture-based susceptibility-guided therapy as a rescue regimen for Helicobacter pylori infection: a randomized controlled trial
Zhe Zhao et al.
Comments (0)