Categories
Change Password!
Reset Password!


For the management of H. pylori-infected treatment-naive patients, two optimized dual regimens were found to have comparable compliance, effectiveness, and safety as the classical dual regimen.
In Helicobacter pylori (H. pylori)-infected individuals who had never received treatment before, two optimized amoxicillin (AMX) and proton pump inhibitors (PPI) dual regimens (Esomeprazole [ESO] 40 mg twice daily or 20 mg thrice daily with AMX 1 g thrice daily for 14 days) demonstrated identical effectiveness, safety, and compliance to the traditional dual regimen (ESO 20 mg + AMX 750 mg four times a day for 14 days). This randomized controlled trial examined the effectiveness, side effects, and patient compliance of three distinct high-dose dual regimens.
In this open-label, prospective, multicenter study, the qualified patients underwent high-dose dual therapy of various regimens with ESO and AMX. ESO 20 mg + AMX 750 mg was given four times a day to group A, ESO 40 mg twice a day + AMX 1 g three times a day was given to group B, and ESO 20 mg + AMX 1 g three times a day was given to group C at random. The three groups' H.pylori elimination rates, adverse events, and patient compliance were contrasted.
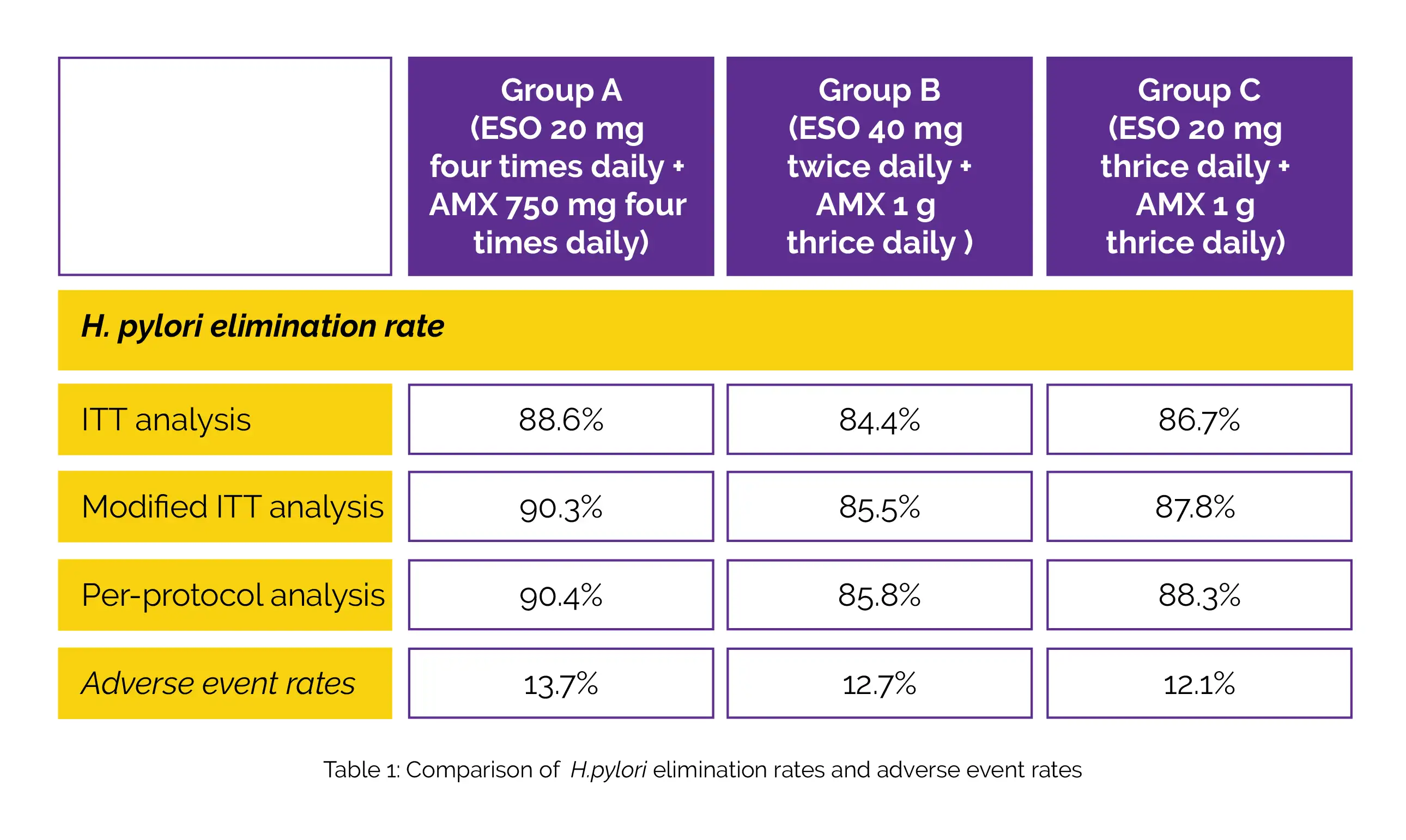
Notably, 945 of 1080 patients that were screened underwent randomization. Table 1 shows adverse event rates in the study groups. According to intention-to-treat (ITT), modified ITT, and per-protocol assessment, the H.pylori elimination rates in groups A, B, and C, are depicted in Table 1:
Antibiotic usage in the past two years lowered group B's elimination effect (ESO 40 mg twice a day, AMX 1 g three times a day). In group B, the adjusted intention-to-treat elimination rates were 81.4% vs. 90.0% for individuals who had or had not previously used antibiotics. The three groups' patient compliance levels were comparable.
Helicobacter
Optimized dual therapy for treatment-naive patients of Helicobacter pylori infection: A large-scale prospective, multicenter, open-label, randomized controlled study
Ying-Ying Han et al.
Comments (0)