Categories
Change Password!
Reset Password!


In patients scheduled to undergo orthognathic surgery, perioperative acetaminophen is beneficial to decrease inpatient opioid analgesia after surgery.
A retrospective cohort study published in 'Journal of Craniofacial Surgery' found perioperative intravenous (IV) acetaminophen to be an effective methodology to minimize inpatient opioid analgesia following orthognathic surgery. Intravenous tranexamic acid and postoperative nausea and vomiting (PONV) control might offer an extra advantage in lowering inpatient opioid intake.
Sarah J Phillips et al. undertook this study to determine the influence of various perioperative factors on inpatient opioid requirements for people undergoing orthognathic surgery. A total of 319 volunteers were segregated into 2 groups: (a) IV acetaminophen group, and (b) No-IV acetaminophen group. In order to compare, the opioids given to volunteers during hospitalization were converted to mean morphine equivalents (MME).
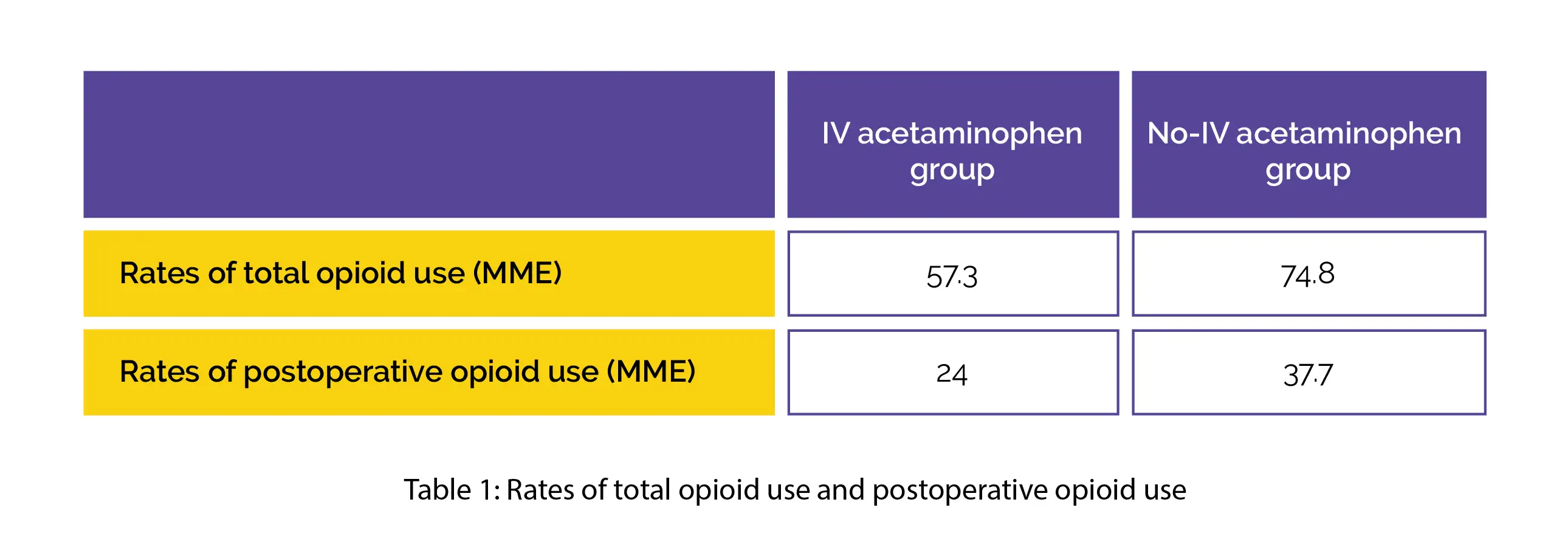
With the aid of a univariate assessment, additional factors that impacted opioid intake, like PONV and tranexamic acid, were recognized. The factors that were noted to exhibit statistical significance were added to the multivariate linear regression model. The IV acetaminophen group exhibited lower rates of total opioid use and postoperative opioid use, as shown in Table 1:
The perioperative prothrombotic agents like tranexamic acid were linked with reduced total and postoperative MME. The multivariate regression assessment depicted that raised PONV led to elevated postsurgery opioid usage. On the other hand, the perioperative acetaminophen was found to diminish total and postoperative quantities.
For alleviating the immediate and long-term risks linked with opioid usage, perioperative IV acetaminophen seems to be valuable. However, additional robust investigations on mechanisms and optimum clinical applications for both tranexamic acid and IV acetaminophen are needed.
Journal of Craniofacial Surgery
Decreasing Inpatient Opioid Use Following Orthognathic Surgery
Sarah J Phillips et al.
Comments (0)