Categories
Change Password!
Reset Password!


Psychological distress is linked to the onset of IBD and inflammation of the mucosa.
In a recent study, patients with inflammatory bowel disease (IBD) experienced markedly elevated levels of stress, anxiety, and depression, which may correlate with specific inflammatory markers in the intestines. Given that stress is a crucial risk factor for the development and progression of IBD, including Crohn's disease (CD) and ulcerative colitis (UC), this study aimed to explore this correlation more deeply.
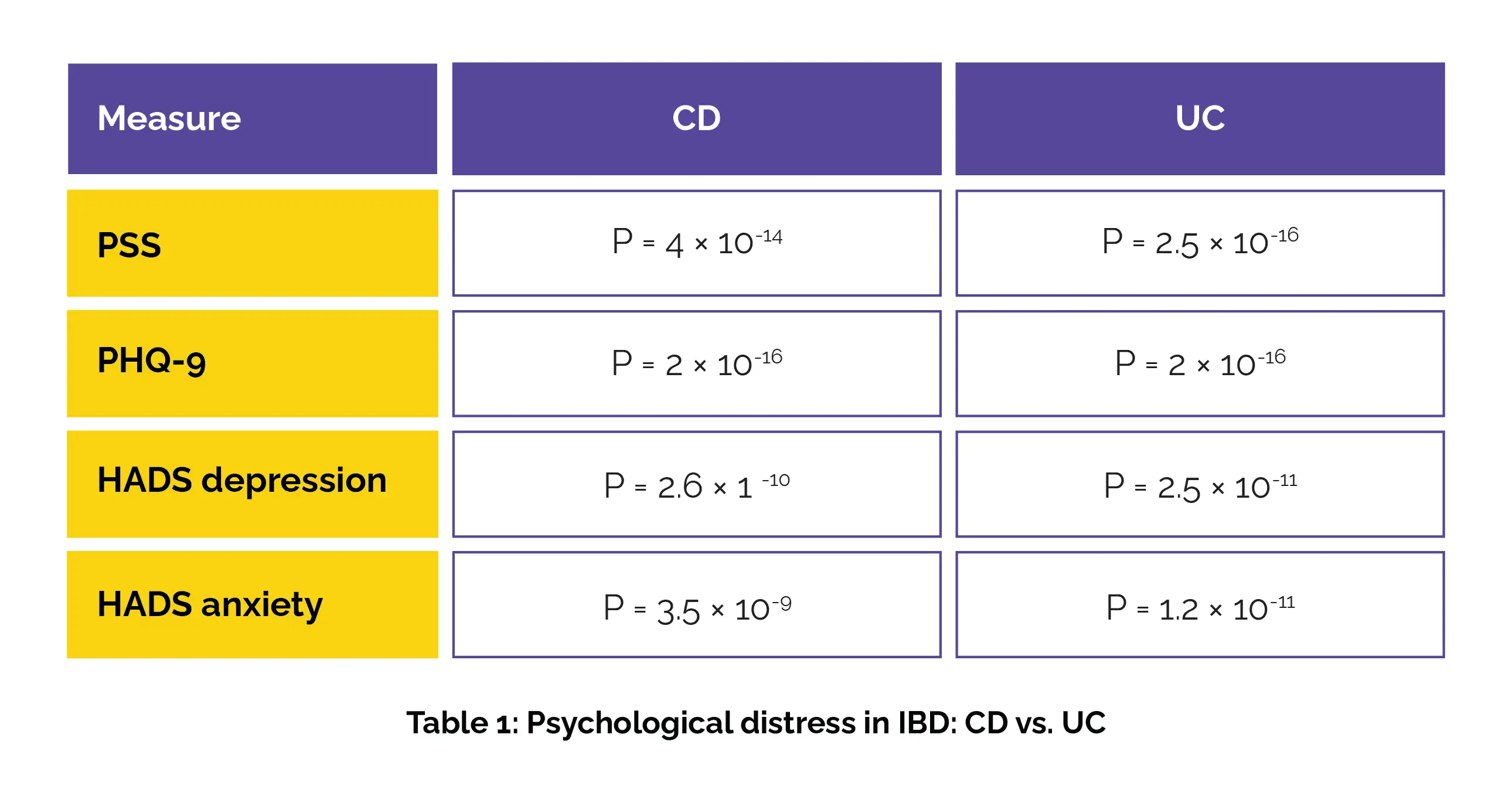
Researchers evaluated stress, anxiety, and depression in 50 patients with CD, 54 with UC, and 100 non-IBD controls. The Patient Health Questionnaire (PHQ-9), Perceived Stress Scale (PSS), and Hospital Anxiety and Depression Scale (HADS) questionnaires were used. Assessment of the link between psychological scores and the expression of IL17A, IL17F, and IL23A genes was carried out in the gut mucosa of IBD-affected patients. Both CD and UC patients exhibited markedly higher scores when compared to the control group, as seen in Table 1 below:
A positive correlation was found between PSS and IL17F mRNA (Spearman's rank correlation coefficient [rs] = 0.43, P = .036), while both HADS depression and anxiety correlated positively with IL23A mRNA levels in the inflamed ileal mucosa of CD patients. To sum up, the occurrence of IBD is connected to psychological distress. In CD patients, higher levels of IL17F and IL23A genes in the ileum are linked to increased stress and anxiety. This suggests a potential interplay between psychological factors and intestinal inflammation.
Inflammatory Bowel Diseases
Psychological Distress Is Associated With Inflammatory Bowel Disease Manifestation and Mucosal Inflammation
Sanja Dragasevic et. al.
Comments (0)