Categories
Change Password!
Reset Password!


Paracetamol and Mannitol injection, in combination with TPVB, can effectively control acute pain and decrease opioid consumption in VATS patients.
In a prospective, double-blind, randomized controlled trial conducted at a leading medical center, Yin Zhou and other investigators have discovered a novel approach to enhance postoperative pain control for patients undergoing video-assisted thoracoscopic surgery (VATS). The combination of Paracetamol and Mannitol injection with thoracic paravertebral block (TPVB) appears to offer significant benefits in acute pain management and may contribute to a diminished need for opioids in patients undergoing VATS.
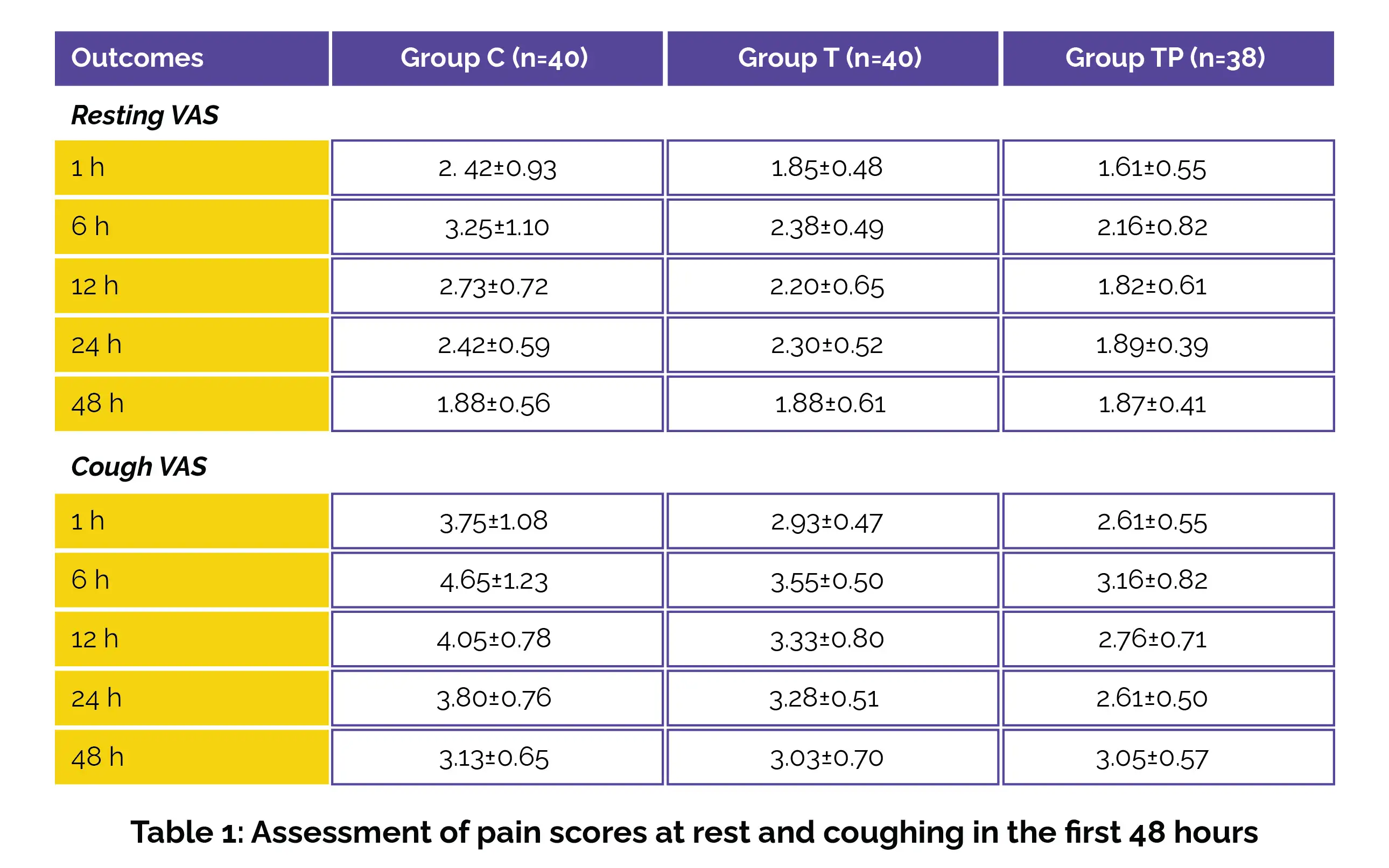
The study focused on the effectiveness of a combination therapy involving Paracetamol and Mannitol injection, coupled with TPVB in post-VATS pain. Those scheduled for VATS were randomized to three groups: General anesthesia group (Group C), TPVB group (Group T), and TPVB combined with Paracetamol and Mannitol injection group (Group TP). The key endpoint was visual analog scale (VAS) scores estimated at rest and during coughing.
Secondary endpoints encompassed the occurrence of adverse events, time to first use of an analgesic pump, total use of Oxycodone in the analgesic pump, urine volume, number of efficient and total analgesic pump compressions in the first 48 hours postoperatively, perioperative Sufentanil use, time to extubation, and length of hospitalization.
Key Findings:
This research has meaningful implications for the field of thoracic surgery and postoperative pain management. The novel approach involving Paracetamol and Mannitol injection plus TPVB has the potential to revolutionize acute pain control and diminish opioid consumption during VATS.
BMC Anesthesiology
Efficacy of postoperative analgesia with intravenous paracetamol and mannitol injection, combined with thoracic paravertebral nerve block in post video-assisted thoracoscopic surgery pain: a prospective, randomized, double-blind controlled trial
Yin Zhou et al.
Comments (0)