Categories
Change Password!
Reset Password!


For reducing pain severity in non-specific low back pain, no high- or moderate-certainty evidence supported the large or medium effectiveness of any pharmacological intervention.
Attention all doctors! Exciting new research has just been published in 'The Cochrane Database of Systematic Reviews,' shedding light on the efficacy and safety of pharmacological interventions for non-specific low back pain (LBP). This comprehensive overview, previously lacking, is set to revolutionize our understanding of back pain treatments.
The study, conducted by a team of dedicated researchers, aimed to summarize the evidence from Cochrane Reviews of systemic pharmacological interventions for adults suffering from non-specific LBP. They meticulously searched the Cochrane Database of Systematic Reviews up until 3 June 2021, scrutinizing reviews of randomized controlled trials (RCTs) to bring us the most up-to-date information.
Two investigators conducted separate evaluations to determine eligibility, gather data, and assess quality of the reviews and certainty of the proof. They utilized the AMSTAR 2 and GRADE tools for this purpose. The review centered on comparing placebos, with the primary outcomes being pain intensity, function, and safety. Overall, 3 reviews focused on people having acute or sub-acute LBP, while 5 reviews encompassed chronic LBP-affected people.
For Acute LBP:
Paracetamol: No significant difference compared to placebo in reducing pain intensity, disability, or increasing the risk of adverse events, with high-certainty evidence supporting this finding.
NSAIDs: Small but significant reduction in pain intensity and disability compared to placebo, supported by moderate-certainty evidence, while the evidence for an increased risk of adverse events was very low-certainty.
Muscle relaxants and benzodiazepines: Moderate-certainty evidence for a small improvement in pain relief and physical function than placebo, but they also had an escalated risk of deleterious events.
Opioids: None of the Cochrane Reviews included in the study aimed to find evidence for acute low back pain and opioid interventions.
Antidepressants: The reviews did not find any evidence for the use of antidepressants in treating acute low back pain.
For Chronic LBP:
Paracetamol: For chronic low back pain, there was no evidence found for the effectiveness of Paracetamol. However, low-certainty evidence supported that NSAIDs showed a small but significant reduction in pain intensity and disability compared to placebo, with no evidence of an increased risk of adverse events at intermediate-term follow-up.
Muscle relaxants and benzodiazepines: The evidence showed that benzodiazepines had a small but significant improvement in pain relief compared to placebo, with low-certainty evidence. However, there was no evidence of a difference between muscle relaxants and placebo regarding the risk of adverse events, also supported by low-certainty evidence.
Opioids: Various opioids' efficacy and safety for treating low back pain have been summarized in Table 1:
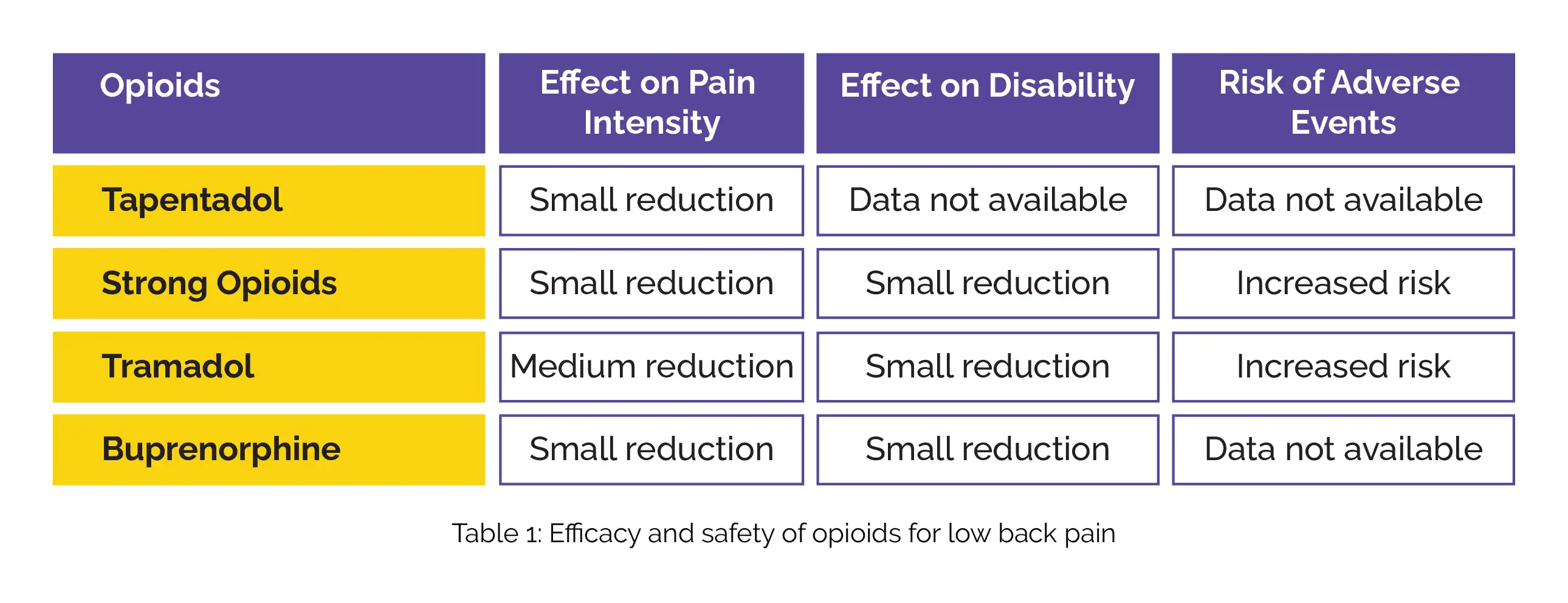
There was a high-certainty evidence supporting Tapentadol's effectiveness in providing a small reduction in pain intensity. Strong opioids also showed a moderate-certainty evidence of small pain reduction. Tramadol demonstrated low-certainty evidence for a medium reduction in pain intensity, while Buprenorphine showed very low-certainty evidence for a small reduction. Regarding disability, strong opioids and Tramadol had a moderate-certainty evidence of a small reduction, and Buprenorphine had a low-certainty evidence of a small reduction.
Considering safety, opioids (all types) showed low-certainty evidence of a small increased risk of adverse events, including nausea, headaches, constipation, and dizziness compared to placebo. The results suggest that Tapentadol and strong opioids might offer some relief for low back pain, but caution is advised due to the increased risk of adverse events associated with opioids.
Antidepressants: Low-certainty evidence showing no significant difference for antidepressants (all types) compared to placebo in reducing pain intensity and disability. Further research is needed to establish their effectiveness in managing low back pain.
In sum up, this cutting-edge study challenges conventional wisdom about back pain meds. It is safe to say that- for acute LBP, stick to NSAIDs and muscle relaxants for modest relief, while Paracetamol might not be as effective as previously believed. For chronic LBP, NSAIDs and opioids could provide some relief, but keep a close eye on the risk of adverse events associated with opioids.
The Cochrane Database of Systematic Reviews
Pharmacological treatments for low back pain in adults: an overview of Cochrane Reviews
Aidan G Cashin et al.
Comments (0)