Categories
Change Password!
Reset Password!


For short- to medium-term anticipation of cognitive deficit in geriatric patients having cognitive deficits, brain FDG PET is beneficial.
In acutely hospitalized geriatric people with newly detected clinically uncertain cognitive impairment, the brain F-fluorodeoxyglucose positron emission tomography (FDG PET) can assist to predict further cognitive/functional deficit and the requirement for assisted living within one to two years. Investigators aimed to assess brain FDG PET for prediction of cognitive impairment, requirement for assisted living, and survival in 96 geriatrics (62 females, 81.4 ± 5.4 years) with cognitive dysfunction.
On the basis of visual inspection by 2 independent readers, FDG PET was classified as "non-neurodegenerative" (DEG-) or "neurodegenerative" (DEG+). Furthermore, each individual PET was tested voxel-wise against the healthy controls. In this study, the total hypometabolic volume served as reader-independent estimate of spatial extent of neuronal degeneration/dysfunction.
The findings at baseline were tested for the link with the alteration in living situation and alteration in vital status twelve to twenty-four months following PET. The link with the annual alteration of the Clinical Dementia Rating Sum of Boxes (CDR-SB) following PET was evaluated in a subsample of 72 volunteers.
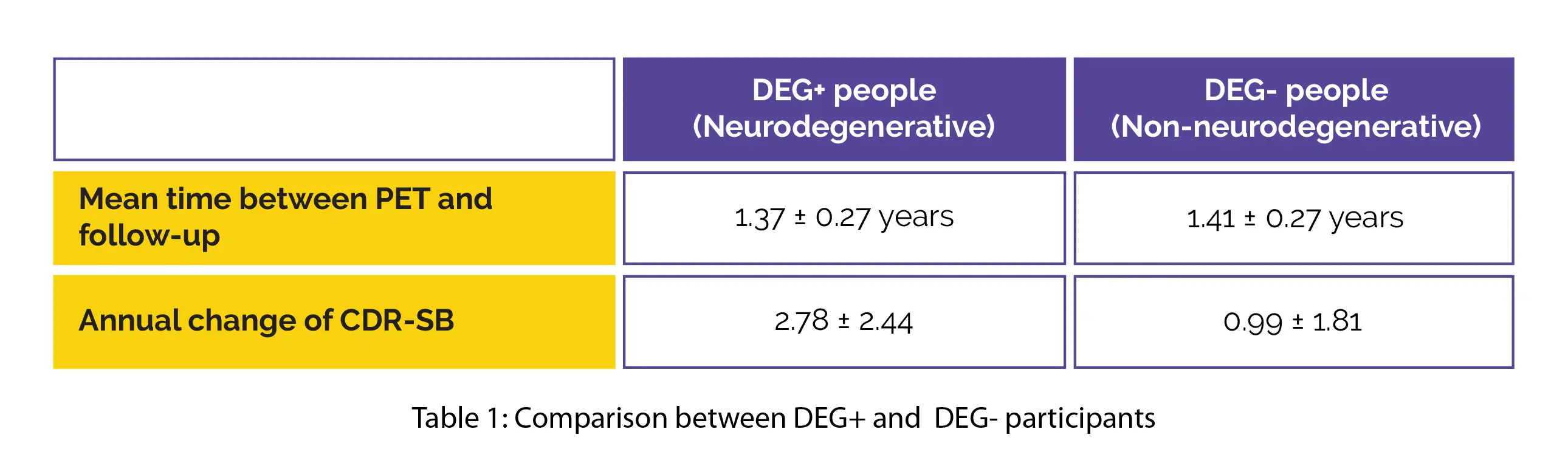
Regarding mean time between PET and follow-up, no inter-group difference was noted. The annual alteration of CDR-SB was greater in DEG+ compared with DEG- people, and it was positively correlated with total hypometabolic volume, as shown in Table 1:
Compared to DEG- people, DEG+ people moved from at home to assisted living considerably earlier. Survival was not related to DEG status or with total hypometabolic volume. Thus, brain FDG PET is valuable to anticipate further cognitive/functional deficits in geriatrics.
Clinical Nuclear Medicine
Brain FDG PET for Short- to Medium-Term Prediction of Further Cognitive Decline and Need for Assisted Living in Acutely Hospitalized Geriatric Patients With Newly Detected Clinically Uncertain Cognitive Impairment
Catharina Lange et al.
Comments (0)