Categories
Change Password!
Reset Password!


For patients dealing with GERD, a novel endoscopic procedure called anti-reflux mucosal valvuloplasty is safe, viable, and efficient.
In a pilot study, anti-reflux mucosal valvuloplasty (ARMV) showed favorable efficacy, feasibility, and safety profile for individuals suffering from gastroesophageal reflux disease (GERD). The study's investigators sought to develop an innovative endoscopic technique for creating a mucosal flap that can prevent acid reflux and address GERD.
The ARMV procedure involves the release and reconstruction of approximately 3/4 circumference of the cardiac mucosa at the lesser curvature side, forming a double-layer mucosal flap. This flap, in conjunction with cardiac scarring, functions to obstruct reflux. Overall, 30 cases that underwent ARMV were examined retrospectively, gathering both subjective and objective data to assess GERD before and after the procedure.
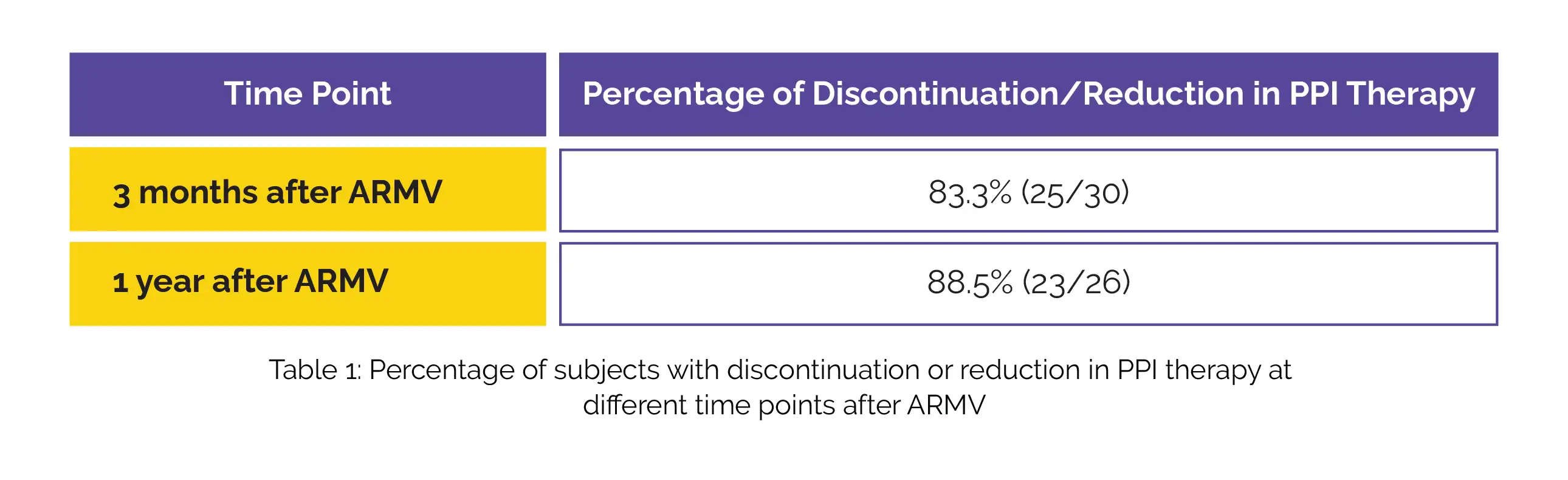
All 30 ARMV procedures were carried out successfully, with a mean operation duration of 72.6±20.3 minutes. One patient experienced post-operative bleeding necessitating endoscopic hemostasis. The mean follow-up period was 28.9±13.9 months. At 3 months and 1 year following ARMV, either reduction or discontinuation in proton pump inhibitor (PPI) therapy was noted in the majority of subjects (Table 1).
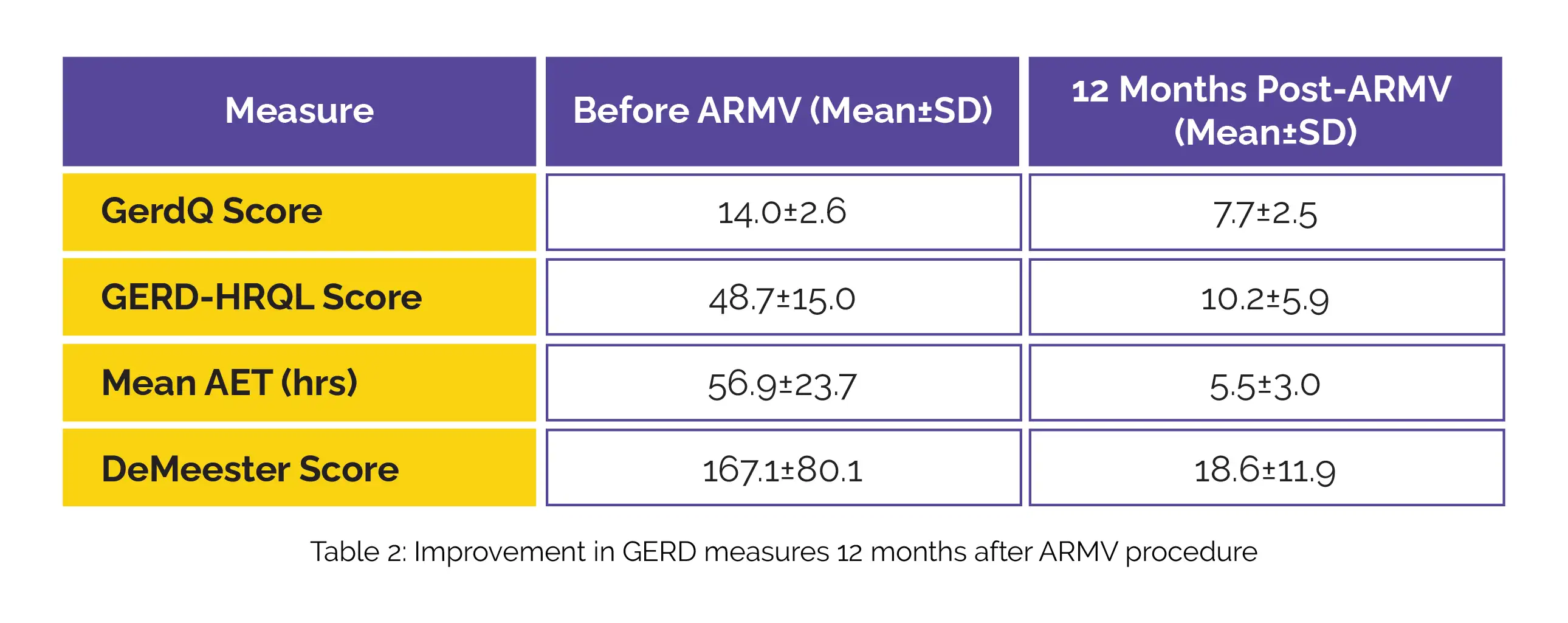
When compared to before ARMV, significant enhancements were observed in GerdQ and GERD-HRQL scores 12 months post-ARMV. Additionally, 11 volunteers underwent 24-hour esophageal pH monitoring before and after ARMV, revealing significant improvements in acid exposure time (AET) and the DeMeester score (Table 2).
Hence, it can be concluded that ARMV offers an effective, feasible, and safe solution for GERD-affected patients. However, further comparative and prospective trials are necessary to establish its role in the realm of endoscopic anti-reflux therapies.
Gastrointestinal Endoscopy
Endoscopic construction of an anti-reflux mucosal barrier for the treatment of gastroesophageal reflux disease, a pilot study
Jiaoyang Lu et al.
Comments (0)