Categories
Change Password!
Reset Password!


The availability of medical information on the web and extensive use of the internet has made patients much more aware of the diseases, symptoms, diagnostic tests, and treatment options. The recent scenario demands that healthcare consumers must have access to all health information and data must be reliable, accurate, and complete. The patient should be in command on how the health information is disclosed, accessed, and used. [1]
To significantly improve both personal and public health care delivery, a robust health information infrastructure was needed which leads to the adoption of electronic personal health record systems (PHRs). Electronic PHRs are a digital application to support patient-centered healthcare by making medical records and other information available digitally to patients, therefore assisting them in health self-management. [2]
The idea of PHR arose from low-technology solutions that people have used for many decades because they required a single place to record their complete medical history which must be accessible. They use to compile paper-based documents that included clinical notes provided by the healthcare providers, health histories, and laboratory reports. [3]
Nowadays, PHR technologies provide countless content-, connectivity-, and collaboration-based features and a useful program for individuals to maintain a lifelong record of clinically sourced and personally reported data from various points of medical care. [4] PHRs allow the patient to keep their health data on hand and accessible for both the consumer and provider while keeping the privacy and security of the data. PHR assist in providing tailored medical care. [5]
PHR: Definition, Components, and Types
PHRs are referred to as a collection of the medical documentation of an individual maintained by themselves or a caretaker, in cases where patients are unable to do so themselves. [5]
According to the Markle Foundation's Connecting for Health collaborative (a public-private endeavor working for interoperable health information infrastructures) PHR can be defined as:
“An electronic application through which individuals can access, manage and share their health information, and that of others for whom they are authorized, in a private, secure, and confidential environment.” [6]
Components of the PHR are lifelong repositories that deliver a wide array of capabilities. The fully accomplished PHR will provide consumers with:
PHRs are broadly divided into 3 main categories:
Steps to Get Started with PHR
To get started with PHR, the following steps are followed:
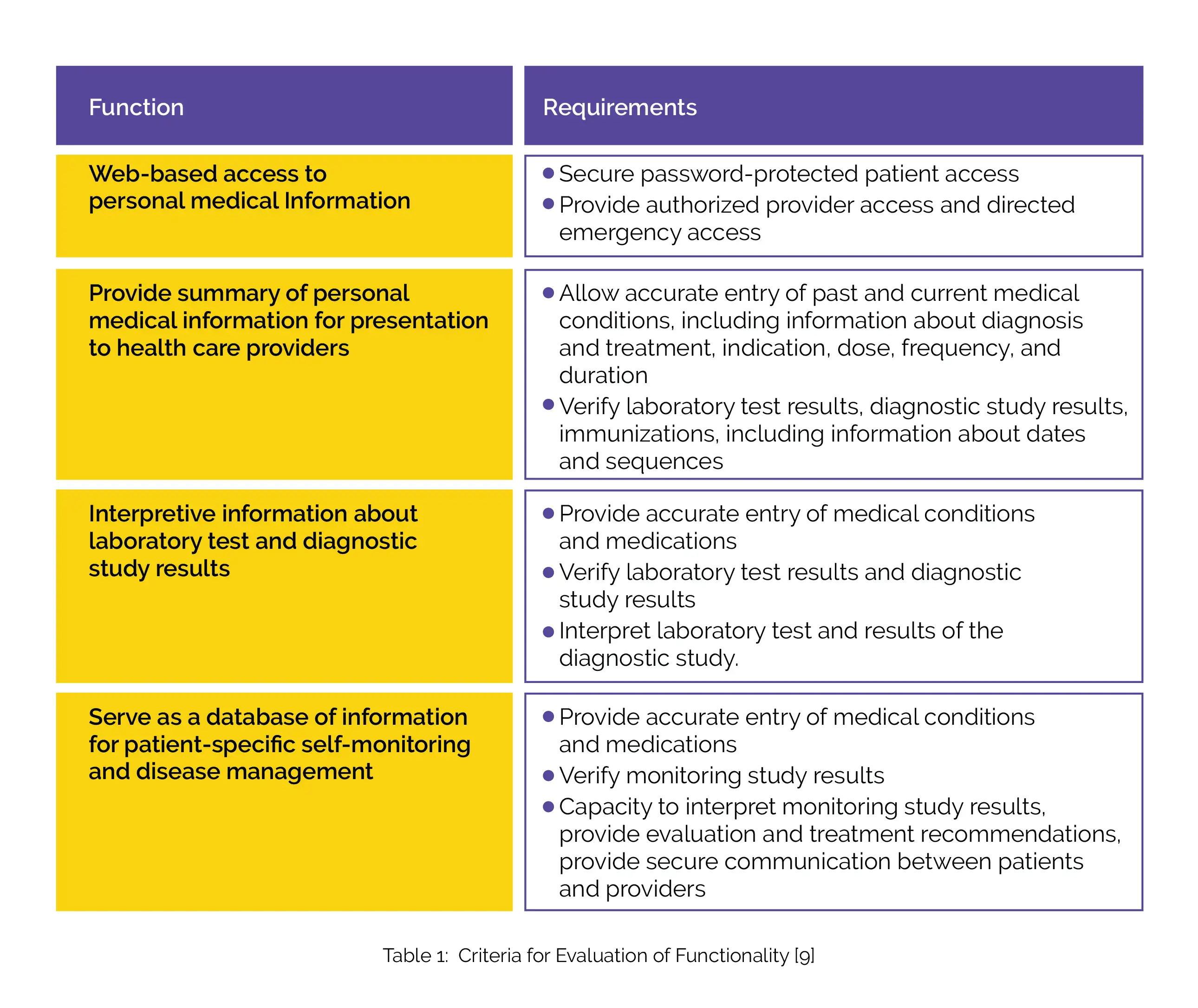
Criteria for maintenance of functionality are shown in the following table 1.
Benefits of PHRs
PHRs have a wide variety of potential benefits for consumers, providers, and the healthcare system that are listed below:
i) Empowerment of patients: PHRs allow the patients to access their health information and supervise their health data. Patients can schedule reminders for health maintenance services via PHR. It is very useful in the management of chronic diseases. It empowers the patients to take active roles in the management and prevention of the disease. [8, 10]

ii) Improved patient-provider relationships: PHRs provide the connection between the patient and physician. It allows documentation of interactions with the patients and conveys timely interpretations of the test results. It allows direct and secure communication between patients and providers. It can make interaction with the patients faster and easier. Providers can be informed earlier if health problems arise via an open line for communication. [8, 11]
iii) Increased patient safety: PHRs identify missed services, provide drug alerts, and get important test results to the patients. It also offers patients timely access to revised medical care plans. [8]
iv) Improved quality of care: PHRs enable extensive care with better coordination between patients and the providers which improve the quality of care. When the patients can track their health over time and have tools to manage their health, their engagement in their health and health care is enhanced. [8, 11]
v) More efficient delivery of care: PHRs avoid duplicative testing and unnecessary services. More efficient communication between patients and physicians is provided. PHRs are a vital resource for patients who are seeking additional health information to make crucial health decisions. [8, 10]

vi) Better safeguards health information privacy: PHRs are more secure than paper records as by providing patients control of access to their records, they offer higher selectiveness in sharing personal health data. Some PHRs are offered by health plans covered by the Health Insurance Portability and Accountability Act of 1996 (HIPAA) Privacy Rule. The HIPAA Privacy Rule applies to these PHRs and safeguards the privacy of the data in them. [8, 12]
vii) Bigger cost savings: As PHRs help avoid duplicative testing, thereby it leads to improved documentation that can decrease malpractice costs. The organization can reduce the costs by using PHR to provide patients with easy access to appointment scheduling applications and electronic prescription refill. [8, 11]
viii) Tracking disease: Patients with chronic illnesses will be able to track their diseases in conjunction with their providers, promoting earlier interventions when they encounter a problem. With the aid of advanced analytics, healthcare providers can better evaluate the risk for future chronic diseases and conditions. [6, 13]
ix) Improved medication: Improved assessment and better clarity of medications to be taken is offered by PHRs. It includes the accurate list of medications a patient might be taking including the name of each drug, its dosage, frequency, and route of administration. This list is used to provide correct medications for patients anywhere within the health care system. [5, 14]

x) Provides reminders: Data from home-monitoring devices can be analyzed and reminds the patient of doctor's appointments. It tracks the vaccination and appointments of the patients and makes the treatment organized. It promotes earlier interventions when the patient encounters a problem. [15, 16]
xi) A powerful tool for daily health management amidst the COVID-19 pandemic: During the COVID-19 pandemic, PHRs have enabled patients to access their cross-hospital medical data and manage it without visiting hospitals, therefore minimizing the risk of infection.[17] PHRs are suitable for the daily management of physical conditions and are suitable as a symptom-tracking tool for COVID-19. Individual habits of enhancing understanding of personal health and the application of PHRs for daily health management are powerful weapons against the rapid spread of infectious diseases. [18]
Practical Examples of PHRs
Challenges and Future Directions
As PHRs exhibit many benefits, they also raise a few concerns. Privacy and accuracy are two of them. Consumers are concerned about the privacy of their health information but if the data is developed precisely, PHRs offer security features and the patient's data can be protected. The accuracy of data entered by the consumers is also one area of concern. But if it is properly developed, this challenge can be overcome. [8] PHR technology offers a platform for patients to maintain a lifelong record of personally reported data and clinically sourced from various points of medical care that is accessible to patients, thus assisting patients in health self-management. [4]
As the consumers want to be more engaged in their healthcare and seek out information online, it will play a key role in the evolving electronically enabled health information environment. The growth of patient self-management tools for remote monitoring will fuel the adoption of PHR. [7] It may accelerate healthcare data exchange as it simplifies the consent models between producers and consumers of healthcare data. [20]
References
Comments (0)